When your pharmacist hands you a pill that looks nothing like the one you’ve been taking for years, it’s normal to pause. Generic drugs are not knockoffs. They’re not cheaper because they’re weaker. They’re cheaper because they don’t carry the marketing costs, patent protections, or brand-name markup. But switching from a brand-name drug to its generic version can still feel unsettling. Here’s what actually happens when you make the switch - and what you should watch for.
Generic drugs work the same way as brand-name drugs
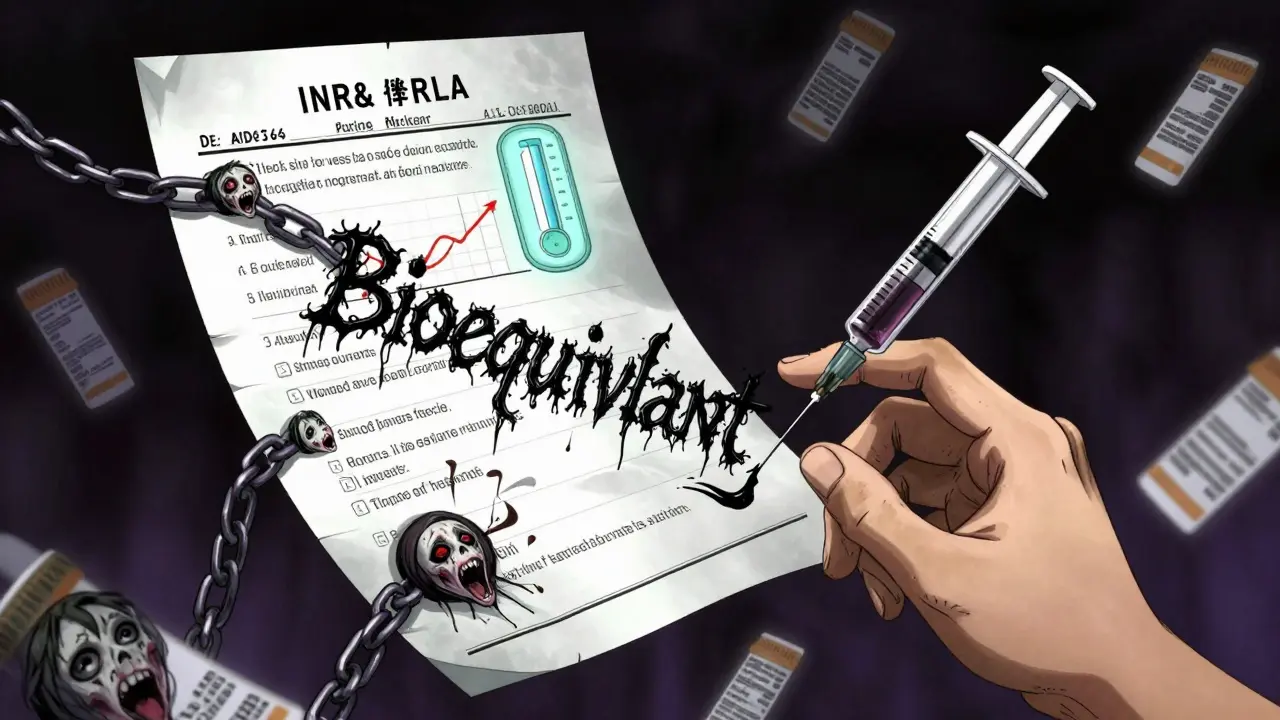
The U.S. Food and Drug Administration (FDA) requires generic drugs to have the exact same active ingredient, strength, dosage form, and route of administration as the brand-name version. That means if you’re taking 10 mg of lisinopril for high blood pressure, the generic version contains the same 10 mg of lisinopril. No more, no less. The FDA doesn’t allow generics to be "close enough." They must prove they deliver the same amount of medicine into your bloodstream at the same rate as the brand. This is called bioequivalence, and it’s tested using real data from blood samples taken after patients take the drug.
Studies back this up. A 2019 analysis of over 2,000 clinical trials published in JAMA Internal Medicine found that generic drugs performed identically to brand-name drugs in 88% of cases. For most people, the switch makes no difference at all. Your blood pressure stays controlled. Your cholesterol stays down. Your depression symptoms stay managed.
Cost savings are real - and massive
The biggest reason to switch? Money. Brand-name drugs can cost hundreds, even thousands, per month. Generics? Often less than $15. According to GoodRx data from September 2023, generics cost 80% to 85% less than their brand-name equivalents. The average patient saves $378 per prescription each year just by switching.
For people on Medicare Part D, the savings are even more dramatic. The 2022 CMS Annual Report found that beneficiaries saved an average of $1,268 annually by choosing generics over brands. That’s not pocket change. That’s groceries, gas, or rent. Maria Rodriguez from Phoenix told ABC15 she was skipping her cholesterol pills because the brand cost $350 a month. The generic? $15. Same effect. She started taking it every day.
And it’s not just about affordability. Kaiser Permanente data shows that patients on generic metformin for diabetes had a 78% adherence rate - compared to just 63% for those on the brand-name Glucophage. When drugs are cheaper, people actually take them.
You’ll notice the difference - but it’s not the medicine
Generics look different. That’s by design. Federal trademark laws require them to look different from the brand-name version. So if your brand-name pill is a blue oval, the generic might be a white round tablet. The shape, color, size, even the imprint code - all can change. That’s not a sign of lower quality. It’s just the law.
Some patients get confused by this. One case reported to the Patient Safety Reporting System involved an 82-year-old woman who took two pills because she didn’t recognize the new generic version of her blood pressure medicine. That’s why pharmacists are required to explain the switch. In 42 states, they must spend 5 to 7 minutes talking to you about the change, what to expect, and what to watch for.
Also, check the Patient Package Insert (PPI) that comes with your prescription. It lists all inactive ingredients - things like dyes, fillers, and preservatives. These don’t affect how the drug works, but they can cause reactions in people with allergies. For example, some generics use FD&C Yellow No. 5 (tartrazine), which can trigger hives or asthma in sensitive people. If you’ve had allergic reactions to medications before, this is worth reviewing.
When you should be cautious
Most drugs are fine to switch. But there are exceptions. The FDA calls them narrow therapeutic index (NTI) drugs. These are medications where even a tiny change in blood levels can cause serious problems - either the drug stops working, or it becomes toxic.
Examples include:
- Levothyroxine (for hypothyroidism)
- Warfarin (a blood thinner)
- Phenytoin and carbamazepine (for seizures)
For these, small differences in how the body absorbs the drug matter more. The American Epilepsy Society found that 12.7% of patients switching between generic antiseizure drugs had breakthrough seizures - compared to just 4.3% who stayed on the same formulation. That’s why many neurologists prefer patients stay on one manufacturer’s version of a generic - not just any generic, but the same one every time. It’s not about brand vs. generic. It’s about consistency.
Similarly, complex delivery systems like inhalers (e.g., Advair Diskus) or topical creams can be tricky. The FDA issued a warning in 2020 about some generic inhalers not dispersing powder the same way as the brand. That can mean less medicine reaches your lungs. For these drugs, don’t assume the generic is interchangeable without checking with your doctor.
What to do after you switch
Don’t just take the new pill and forget about it. Monitor yourself for the first two weeks.
Keep a simple log:
- Are your symptoms the same? (e.g., chest pain, headaches, mood swings)
- Do you feel different? (e.g., dizziness, nausea, fatigue)
- Any new side effects?
For certain conditions, track specific numbers:
- Diabetes: Check fasting blood sugar. If it jumps more than 20 mg/dL from your usual range, call your doctor.
- Blood thinners (warfarin): Watch your INR levels. A change of more than 0.5 units could mean your dose needs adjusting.
- Depression or anxiety: Use a simple scale like PHQ-9 or GAD-7. If your score drops by 3 or more points, talk to your provider.
If something feels off, don’t assume it’s "all in your head." It might be the inactive ingredients. Or it might be that your body adapted to a specific manufacturer’s version. Either way, report it. You can call the FDA’s Medication Errors Reporting Program at 1-800-FDA-1088. Your feedback helps improve safety.
What’s changing in the future
The FDA is pushing for better labeling. By 2025, generic drug labels will be required to clearly list all potential allergens - not just bury them in fine print. That’s a big step.
Also, more complex generics are coming. Biosimilars - the next generation of generics for biologic drugs like Humira - are now entering the U.S. market. They’re not exact copies (biologics are too complex), but they’re designed to work the same way. And they’re already cutting costs by 15% to 30%.
By 2030, experts predict 95% of all prescriptions will be filled with generics. That’s not because brand-name drugs are disappearing. It’s because the system is working. Generics are safe, effective, and affordable.
Bottom line: Switch - but stay aware
For most people, switching to a generic drug is a smart, safe move. You’ll save hundreds or even thousands of dollars each year with no loss in effectiveness. The science is clear. The data is solid. The FDA stands behind it.
But don’t be passive. Know what you’re taking. Check the label. Track your symptoms. Talk to your pharmacist. If you’re on a high-risk medication like warfarin or levothyroxine, ask your doctor if you should stick with one specific generic brand. And if something feels wrong after the switch - speak up. Your body knows when something’s off. Listen to it.
Generics aren’t second-rate. They’re smart medicine. And if you’re paying less while getting the same results - that’s not a compromise. That’s progress.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards for quality, strength, purity, and stability as brand-name drugs. They must prove they work the same way in the body. Millions of people take generics every day without issue. The FDA monitors them just as closely as brand-name drugs.
Why do generic pills look different?
Federal trademark laws require generic drugs to look different from the brand-name version. That means different color, shape, size, or imprint. It has nothing to do with effectiveness. It’s just to avoid confusion and protect the brand’s trademark. Your pharmacist should explain this when you get the new prescription.
Can I switch back to the brand if the generic doesn’t work?
Yes. If you notice changes in how you feel - like new side effects, reduced effectiveness, or unusual symptoms - contact your doctor. They can write a prescription that says "dispense as written" or "no substitutions." Your insurance may require prior authorization, but your health comes first. Don’t suffer through a medication that doesn’t work for you.
Are all generics the same, or do different manufacturers make a difference?
All generics approved by the FDA are bioequivalent to the brand. But for a small group of drugs - especially those with a narrow therapeutic index - some patients respond better to one manufacturer’s version than another. This isn’t about quality. It’s about subtle differences in how the drug is absorbed due to inactive ingredients or manufacturing processes. If you’re on a critical medication like levothyroxine or an antiseizure drug, ask your doctor if you should stick with the same generic brand every time.
What if I have allergies? Should I worry about generic drugs?
Yes, check the inactive ingredients. Generics can use different dyes, fillers, or preservatives than the brand. For example, some contain FD&C Yellow No. 5, which can trigger reactions in people allergic to tartrazine. Always read the Patient Package Insert that comes with your prescription. If you’re unsure, ask your pharmacist to check the ingredients against your known allergies.

The FDA's bioequivalence standards are rigorous, but real-world variability still exists in dissolution profiles across manufacturers. I've seen patients on levothyroxine whose TSH levels fluctuated after switching generics-not because the active ingredient changed, but because the excipients altered absorption kinetics. Documented cases exist. Don't dismiss anecdotal evidence just because it doesn't fit the narrative.
Let’s be honest-this whole generic drug push is just corporate greed dressed up as public health. Big Pharma doesn’t want you saving money; they want you dependent on their patented products. But now that generics are everywhere, who’s really controlling the supply chain? China produces 80% of the active pharmaceutical ingredients. Do you really think your blood pressure pill is safe when it’s made in a factory with no FDA oversight? The FDA inspects less than 2% of foreign plants. This isn’t medicine-it’s a global gamble with your life.
There is a fundamental misunderstanding in the public perception of generics. The FDA’s requirement for bioequivalence is not merely ‘close enough’-it’s statistically proven equivalence within a 90% confidence interval for Cmax and AUC, with limits of 80–125%. Any claim that generics are ‘inferior’ is scientifically baseless. Furthermore, the assertion that inactive ingredients cause widespread adverse reactions is misleading; true allergies to excipients like tartrazine affect less than 0.1% of the population. Please stop conflating personal anecdotes with clinical evidence.
I’m from Kenya and we rely on generics here-no choice, really. But what I’ve seen is that when pharmacists take the time to explain the switch, patients trust it. We don’t have the luxury of brand-name drugs, so we’ve learned to read labels, ask questions, and track symptoms. It’s not about trust in corporations-it’s about trust in your own body and your pharmacist. If you’re worried, keep a journal. Write down how you feel. Talk to your provider. That’s the real power move here.
While the statistical data presented is commendable, one must exercise due diligence in the context of pharmaceutical manufacturing standards across jurisdictions. The global supply chain for active pharmaceutical ingredients remains susceptible to regulatory arbitrage, and the absence of consistent Good Manufacturing Practice enforcement in certain regions introduces an element of systemic risk. It is therefore prudent to maintain vigilance, particularly in the context of medications with narrow therapeutic indices.
My grandma switched to generic lisinopril and didn’t even notice. She was scared at first because the pill looked like a Pepto-Bismol tablet. But she checked her BP every day for two weeks-same numbers, same energy. She’s been saving $300/month since. If your doctor says it’s safe, give it a shot. Worst case? You go back. Best case? You keep your lights on.
Check the PPI. Always. Tartrazine and lactose are the usual suspects.
Oh sure, the FDA says it’s fine. But why do you think they pushed this so hard right after the 2020 pandemic? Coincidence? Nah. They knew people were broke. Now you’re hooked on cheap pills made in some basement lab while the real doctors get paid off by Big Pharma. And don’t even get me started on the ink on the pills-it’s coded. They’re tracking you. That’s why the shape changes. So you don’t notice you’re being dosed differently.
generic drugs r a scam. the fda is corrupt. my friend took generic adderall and turned into a zombie. the fillers are laced with microchips. they want us docile. also, why do all the pills look like they were made by a 5-year-old? because they are. the chinese government owns the factories. and the color changes? that’s the government’s way of telling you when to stop taking it. i saw it on a forum. trust me, i know.