Managing diabetes isn’t about cutting out all the foods you love-it’s about making smarter choices that keep your blood sugar steady and your body healthy. If you’re trying to figure out what to eat and what to skip, you’re not alone. Millions of Americans with diabetes use simple, proven strategies every day to stay in control. The key isn’t perfection. It’s consistency.
Start with the Plate Method
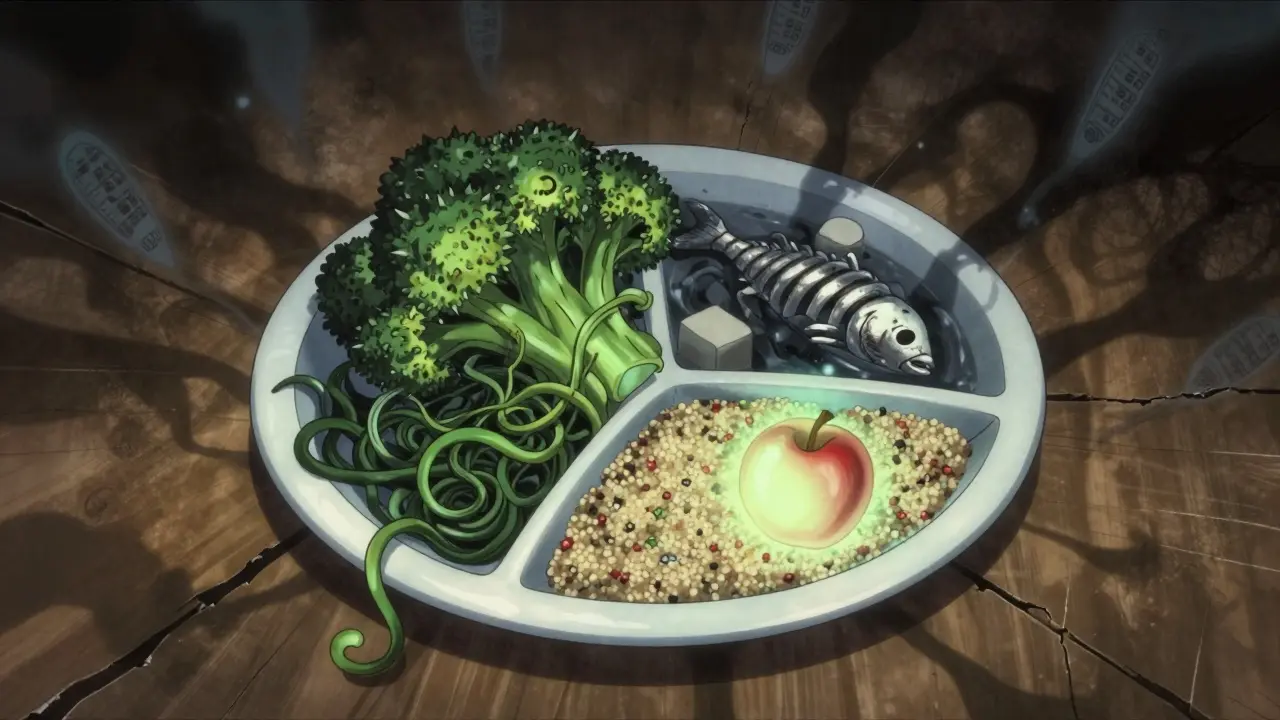
The easiest way to build a diabetes-friendly meal doesn’t involve counting calories or tracking carbs. It’s called the Diabetes Plate Method. Developed by the American Diabetes Association and backed by the CDC, this visual tool turns your dinner plate into a guide for balanced eating. Here’s how it works: Take a 9-inch plate-about the size of a standard dinner plate or a business envelope. Divide it into three sections:- Half the plate: Non-starchy vegetables. Think broccoli, spinach, carrots, bell peppers, zucchini, mushrooms, and green beans. These are low in carbs and high in fiber, so they fill you up without spiking blood sugar.
- One-quarter of the plate: Lean protein. Choose skinless chicken, turkey, fish (especially salmon or sardines), tofu, eggs, or beans. These help you stay full and support muscle health without adding sugar.
- The last quarter: Healthy carbohydrates. Go for whole grains like quinoa or barley, starchy vegetables like sweet potatoes, or a small piece of fruit. This is where portion control matters most.
Want to know how much that is? A 3-ounce portion of meat is about the size of your palm. One tablespoon of peanut butter is the tip of your thumb. One cup of fruit fits in your fist. These visual cues make it easy to eat right-even when you’re not reading labels.
Foods That Help You Stay in Control
Not all carbs are bad. In fact, the Dietary Guidelines for Americans recommend that 50-60% of your daily calories come from carbohydrates-just make sure they’re the right kind.- Non-starchy vegetables: These are your best friends. A cup of cooked broccoli has only 6 grams of carbs and 5 grams of fiber. That means your body digests it slowly, keeping blood sugar steady.
- Fatty fish: Salmon, mackerel, and sardines are packed with omega-3s, which reduce inflammation and lower heart disease risk-something people with diabetes need to watch closely. Aim for at least two servings a week.
- Legumes: Beans, lentils, and chickpeas are high in fiber and protein. A half-cup of black beans has 20 grams of carbs, but 7 grams of fiber, so the net impact on blood sugar is much lower.
- Whole grains: Swap white rice for brown rice, white bread for whole-wheat bread, and regular pasta for barley or quinoa. These take longer to break down, so your blood sugar doesn’t spike as fast.
- Healthy fats: Avocados, nuts, seeds, and olive oil don’t raise blood sugar. They also help your body absorb nutrients and keep you satisfied longer.
- Low-fat dairy: Milk, yogurt, and cheese can fit in your plan-but watch out for added sugar. Some "non-fat" yogurts have more sugar than ice cream. Always check the label.
One real-life example: A breakfast of scrambled eggs with spinach and tomatoes, a slice of whole-wheat toast, and a small apple keeps blood sugar stable until lunch. No crashes. No cravings.
Foods to Limit or Avoid
Some foods might taste good, but they’re not your allies when you have diabetes. These are the ones to cut back on-or skip entirely.- Refined grains: White bread, white rice, and regular pasta are stripped of fiber and digest fast. One slice of white bread can raise blood sugar as much as a candy bar.
- Sugary drinks: Soda, sweetened tea, fruit punch, and even 100% fruit juice spike blood sugar quickly. A single 12-ounce can of soda has 39 grams of sugar. That’s more than the daily limit for added sugar recommended by the American Heart Association.
- Processed meats: Bacon, sausage, deli meats, and hot dogs are high in sodium and preservatives. Studies link them to higher insulin resistance and heart disease risk.
- Added sugars: Candy, cookies, cakes, pastries, and sweetened cereals are pure sugar with little to no nutrition. Even "sugar-free" products can contain sugar alcohols that still affect blood sugar.
- High-fat dairy: Whole milk, full-fat cheese, and cream are loaded with saturated fat. That’s not good for your heart-and people with diabetes are already at higher risk.
- Fried foods: Fried chicken, French fries, and onion rings are double trouble: high in carbs and unhealthy fats. Both raise blood sugar and inflammation.
Here’s a common mistake: People think "low-fat" means healthy. But many low-fat yogurts, salad dressings, and granola bars replace fat with sugar. Always read the ingredient list. If sugar is one of the first three ingredients, it’s probably not a good choice.

Timing Matters Just as Much as What You Eat
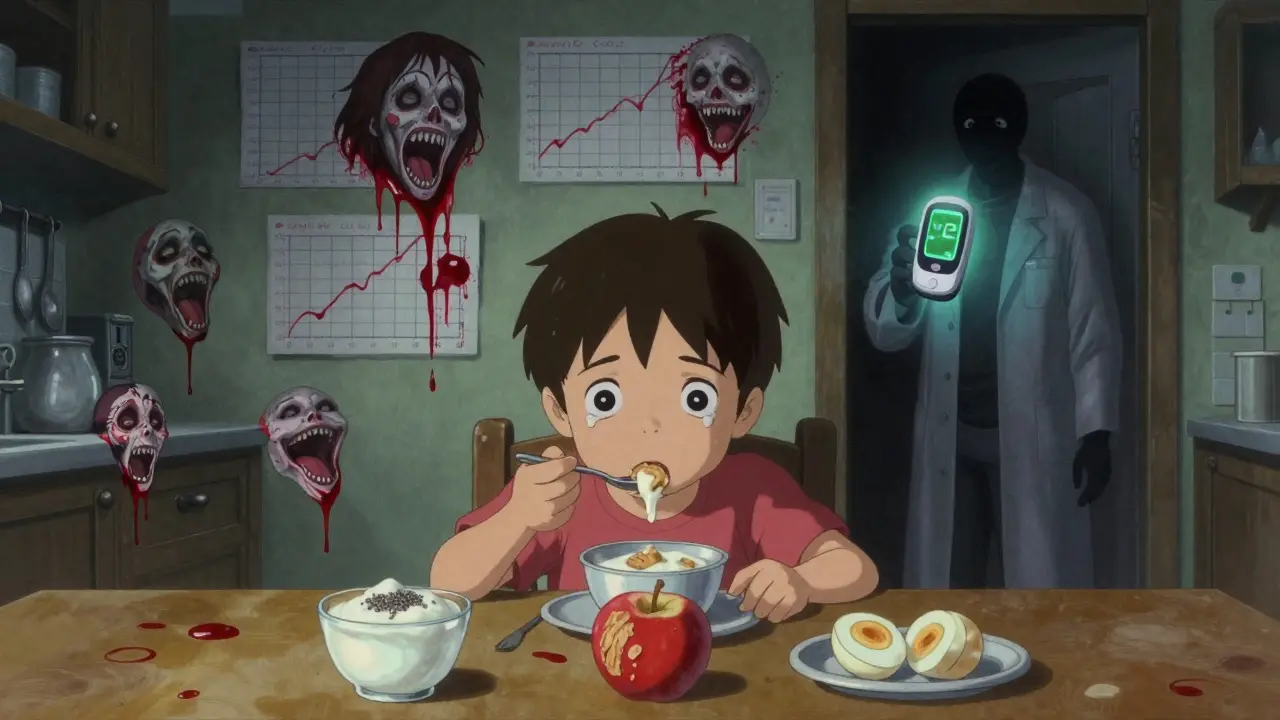
It’s not just about what’s on your plate-it’s when you eat it. The American Diabetes Association recommends eating meals and snacks at regular times. Try to space them 2-3 hours apart. This gives your body time to bring blood sugar back down before the next meal. For example, if you eat breakfast at 7 a.m., aim for lunch at 1 p.m. and dinner at 7 p.m. Skipping meals can cause blood sugar to drop too low, then rebound too high when you finally eat. If you’re active, plan a small snack before or after exercise. A handful of almonds or a piece of fruit can prevent low blood sugar during a walk or workout.For kids with Type 2 diabetes, the University of Florida Health recommends three small meals and three snacks a day to support growth while keeping blood sugar steady.
Real Meals That Work
You don’t need fancy recipes. Simple, balanced meals are the most sustainable.- Breakfast: Greek yogurt (unsweetened) with chia seeds and blueberries, plus a boiled egg.
- Lunch: Grilled chicken salad with mixed greens, cherry tomatoes, cucumbers, olive oil, and vinegar. Add a small orange on the side.
- Dinner: Baked salmon, roasted Brussels sprouts, and ½ cup of quinoa.
- Snack: A small apple with 1 tablespoon of almond butter.
These meals follow the plate method without needing a calculator. And they’re easy to adapt for cultural preferences. Want rice? Use brown rice. Want beans? Use black beans. The structure stays the same.
What About Carbs?
You’ve probably heard carbs are bad. That’s not true. It’s about the type and amount. Most adults with diabetes can handle 45-60 grams of carbs per meal. But that varies by person. If you’re using a continuous glucose monitor (CGM), you’ll see exactly how your body responds to different foods. That’s the most powerful tool you have. The 2022 Nutrition Consensus Report from the ADA says meal plans should be personalized. What works for your neighbor might not work for you. Track your blood sugar after meals for a week. Write down what you ate and how you felt. You’ll start to notice patterns.Challenges and How to Overcome Them
Eating well isn’t always easy. Many people face real barriers:- Cultural foods: Traditional meals from your heritage might include rice, fried foods, or sugary sauces. You don’t have to give them up-just adjust. Use less rice, add more vegetables, and swap frying for baking.
- Eating out: Choose grilled over fried. Ask for dressings on the side. Split an entree with someone. Most restaurants now list carb counts online.
- Food insecurity: About 23% of adults with diabetes struggle to afford healthy food. Frozen vegetables, canned beans (rinsed to remove salt), and eggs are affordable, shelf-stable options that fit the plate method.
The goal isn’t to eat perfectly every day. It’s to make better choices most of the time. One unhealthy meal won’t ruin your progress. But consistent, balanced eating over months? That’s what lowers your A1C by 0.3 to 2.0 percentage points-enough to reduce your risk of nerve damage, kidney disease, and heart problems.
Tools to Help You Stay on Track
You don’t have to do this alone.- The Diabetes Food Hub (from the ADA) lets you build free meal plans and save recipes. You can drag and drop meals into a weekly calendar.
- Continuous glucose monitors (CGMs) show you real-time effects of food. Many insurance plans now cover them.
- Virtual coaching: The CDC’s Diabetes Prevention Program offers free online sessions with dietitians who specialize in diabetes.
These aren’t luxuries. They’re practical tools used by thousands of people every day to live better with diabetes.
Can I still eat fruit if I have diabetes?
Yes, absolutely. Fruit contains natural sugars, but it also has fiber, vitamins, and antioxidants. Choose whole fruits like apples, berries, oranges, and pears instead of juice. A small piece of fruit or ½ cup of berries counts as one serving. Eat them with protein or fat-like a handful of nuts-to slow down sugar absorption.
Are artificial sweeteners safe for people with diabetes?
Most artificial sweeteners like stevia, sucralose, and aspartame don’t raise blood sugar. But some studies suggest they might affect appetite or gut health over time. Use them sparingly. Better yet, train your taste buds to enjoy food without added sweetness. Over time, you’ll crave less sugar.
How often should I check my blood sugar when changing my diet?
If you’re adjusting your meals, check your blood sugar before and 2 hours after eating for about a week. This helps you see how different foods affect you. You don’t need to check forever-just long enough to learn your body’s patterns. Once you know what works, you can check less often.
Can I lose weight with a diabetic meal plan?
Yes, and it’s one of the most powerful benefits. A balanced meal plan that focuses on vegetables, lean protein, and healthy fats naturally reduces calorie intake without leaving you hungry. Many people with Type 2 diabetes see improved blood sugar control-and even remission-when they lose 5-10% of their body weight through consistent eating and movement.
What if I don’t like vegetables?
Start small. Try roasting them with olive oil and garlic-it brings out natural sweetness. Blend spinach into smoothies. Add finely chopped veggies to soups, omelets, or pasta sauce. You don’t need to love kale to benefit from it. Just get a little more in each day. Over time, your taste buds adapt.
If you’re just starting out, pick one change to focus on. Maybe it’s swapping soda for sparkling water. Or adding a vegetable to every meal. Small steps add up. You don’t need to overhaul your life overnight. You just need to keep moving forward.

Let me cut through the noise - this plate method is the only thing that actually works. No counting. No apps. Just look at your plate. Half veggies, quarter protein, quarter carbs. Done. I’ve helped 3 family members get their A1C under 7 with this and zero willpower. It’s not magic. It’s math. Your body doesn’t care about labels. It cares about volume and density. Eat like your life depends on it - because it does.
Stop buying "diabetic-friendly" junk. That’s just sugar with a fancy name. Real food doesn’t need a label.
This is SO good 😊 I’ve been using the plate method for 8 months and my A1C dropped from 8.2 to 5.9! I didn’t even realize I was eating so many processed carbs until I started using my hand as a measuring tool 🤯 I literally just started with one meal a day - breakfast - and now it’s automatic. You don’t need to be perfect, just consistent. And yes, frozen veggies are a lifesaver 💪❤️
People forget that timing matters just as much as what you eat. Skipping meals makes your liver dump glucose like crazy. I used to skip lunch because I was busy. My afternoon sugars would spike then crash. Now I eat every 3 hours. Snack is a hard boiled egg or a few almonds. No drama. No hunger. Just steady. And yeah the plate method works but only if you stick to it. No exceptions.
Also if you’re using a CGM you’ll see how fast white rice turns your numbers into a rollercoaster. Brown rice is slow. Real slow.
It’s fascinating how the body responds not just to macronutrients but to rhythm. The circadian regulation of insulin sensitivity means that eating the same meal at 7 a.m. versus 9 p.m. can produce entirely different glycemic outcomes. This isn’t just diet - it’s chronobiology. And yet we treat nutrition like a static equation when it’s a dynamic conversation between our cells and the environment.
Why do we assume that all carbs are equal when the glycemic index varies wildly even within the same food group? A ripe banana versus an unripe one. White rice versus wild rice. The difference isn’t just in the label - it’s in the molecular structure, the fiber matrix, the phytonutrient profile. We’ve reduced nutrition to a numbers game while ignoring the living complexity of food. The plate method works because it respects that complexity without requiring a PhD to understand it. It’s elegant. It’s humble. And it’s deeply biological.
But then again - why do we need a method at all? Why not just return to eating whole foods the way our ancestors did? The real question isn’t how to manage diabetes - it’s how we let ourselves get this far out of sync with our evolutionary biology in the first place.
And yet - I know the system we live in doesn’t reward that kind of thinking. It rewards convenience. It rewards profit. It rewards the illusion of control through apps and metrics. So maybe the plate method is the only real rebellion left - eating slowly. Eating locally. Eating simply. Eating like you’re still part of nature and not just a data point in a corporate dashboard.
So yes. Half plate. Quarter protein. Quarter carbs. And maybe - just maybe - eat in silence once in a while. Notice the taste. Feel the texture. Remember that food isn’t fuel. It’s memory. It’s culture. It’s love. And it’s medicine.
But I’ll stop now. I’m getting philosophical again.
My mom used to cook rice every day but she always added lentils and spinach. She didn’t know about plate method but she knew how to feed us. Now I do the same. Brown rice with dal and bitter gourd. Simple. Cheap. Works. No fancy apps. Just food that was made by hands not factories. I wish more people in America knew this. We don’t need to reinvent the wheel. We just need to remember what our grandmas already knew.
Also roasted cauliflower with turmeric and garlic is the best snack ever. Try it.
Who told you the ADA is trustworthy? They take money from big food companies. That plate method? It’s designed to keep you buying their processed "whole grain" bread and sugar-free yogurt. They want you dependent on their system. Real food doesn’t need a USDA stamp. Real food doesn’t come in a box. You think they want you to cure diabetes? No. They want you to manage it. Forever. With their products. Read the fine print on those "diabetic-friendly" labels. Sugar alcohols. Modified corn starch. All of it’s a scam. Eat meat. Eggs. Butter. Broccoli. That’s it. No carbs. No lies. No ADA.
I get where the ADA is coming from but honestly I think the real issue is that most of us are just tired. We’re not lazy. We’re exhausted. Trying to eat right while working two jobs, raising kids, and dealing with insurance headaches? It’s a lot. The plate method helps because it doesn’t ask you to be perfect. It just asks you to try. One meal. One day. One vegetable at a time. That’s enough.
And if you can’t afford fresh veggies? Frozen ones are just as good. Canned beans? Rinse them. Done. You’re not failing. You’re surviving. And that’s still victory.
For those asking about fruit - yes, you can eat it. But pair it. Apple with peanut butter. Berries with Greek yogurt. The fat and protein slow absorption. I’ve seen patients reverse prediabetes just by swapping out juice for whole fruit and adding a protein source. No meds needed. Just awareness. Also - if you’re using a CGM, track for 7 days. You’ll be shocked at how different your body responds compared to your friend’s. Personalization is key. Not dogma.
You people are so naive. This isn’t about food. It’s about control. They want you thinking it’s your fault you’re diabetic. That if you just ate better you’d be fine. But what about the pesticides? The water fluoridation? The glyphosate in your bread? The government is using diabetes to push you into the wellness-industrial complex. Buy their supplements. Subscribe to their apps. Pay for their coaching. Meanwhile the real cause? Vaccines. GMOs. 5G. You think this is about carbs? It’s about population reduction. And you’re all eating it up - literally. Wake up. Eat meat. Don’t touch carbs. Don’t trust anyone who says otherwise.