Interchangeable Biosimilars: What They Are and How They Compare to Generics
When you hear interchangeable biosimilars, a type of biologic medication approved by the FDA to be substituted for a brand-name biologic without the prescriber’s involvement. Also known as biosimilar substitutes, these drugs are not generics—they’re complex, living-cell-derived treatments that mimic the effects of expensive biologics like Humira or Enbrel. Unlike traditional generics, which copy simple chemical formulas, interchangeable biosimilars must prove they produce the same clinical results, with no meaningful difference in safety or effectiveness. That’s why the FDA requires extra testing—studies on immune response, dosing, and long-term outcomes—before granting interchangeability status.
Interchangeable biosimilars relate closely to therapeutic equivalence, the standard that ensures a drug performs the same way in the body as its reference product. This concept is the backbone of generic drug substitution, but with biosimilars, it’s even stricter. For example, while a generic version of warfarin might need close INR monitoring after a switch, an interchangeable biosimilar for rheumatoid arthritis must show zero difference in how it affects disease progression or side effects across thousands of patients. That’s why not all biosimilars are interchangeable—only those that pass the highest bar.
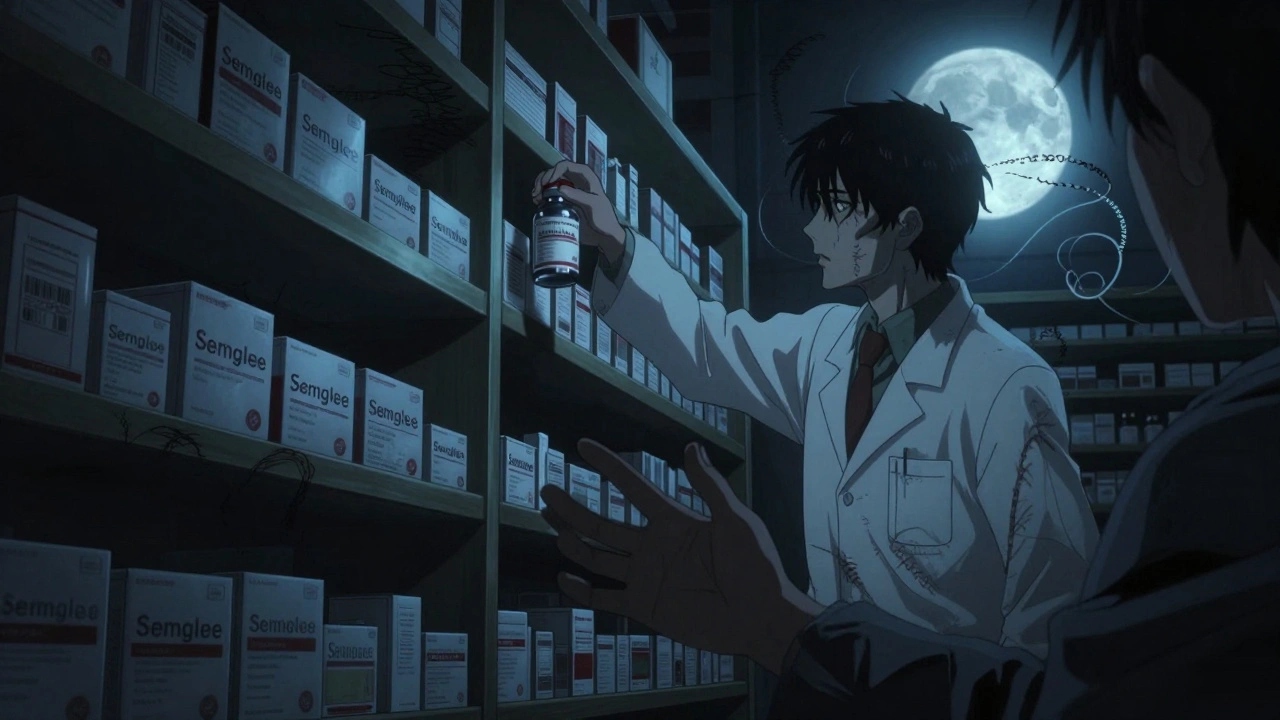
These drugs also connect to biologic medications, complex proteins made from living cells, used to treat autoimmune diseases, cancer, and chronic conditions. Unlike small-molecule drugs, biologics can’t be exactly copied—they’re too big, too fragile, and too sensitive to manufacturing changes. That’s why biosimilars are called "similar," not "identical." Even tiny differences in how they’re made can affect how your body reacts. That’s why pharmacists and doctors watch for subtle shifts in symptoms after switching, especially with drugs like insulin or blood thinners.
Many people assume all cheap versions of brand-name drugs are the same. But interchangeable biosimilars aren’t just lower-cost generics—they’re a new category of medicine designed to bring advanced treatments within reach. They’re changing how patients with chronic conditions like Crohn’s, psoriasis, or diabetes manage their care. And with more hitting the market every year, understanding what makes them different—and when they can be safely swapped—is becoming essential.
Below, you’ll find real-world insights from posts that dig into how these drugs are approved, how they compare to traditional generics, what doctors look for when switching, and why some patients still hesitate—even when the science says it’s safe.
When Can Biosimilars Be Automatically Substituted? Understanding Interchangeability in the U.S.
Interchangeable biosimilars can be automatically swapped for brand-name biologics at the pharmacy level in the U.S., but only under strict FDA rules and varying state laws. Learn how they work, who can substitute them, and what patients need to know.
read more