When you walk into a pharmacy to pick up your insulin or rheumatoid arthritis medication, you might not realize that what you’re handed could be a biosimilar-and that it might have been swapped in without your doctor’s knowledge. This isn’t a glitch in the system. It’s the result of a specific FDA designation called interchangeability. And it’s changing how millions of Americans access life-saving biologic drugs.
What Exactly Is an Interchangeable Biosimilar?
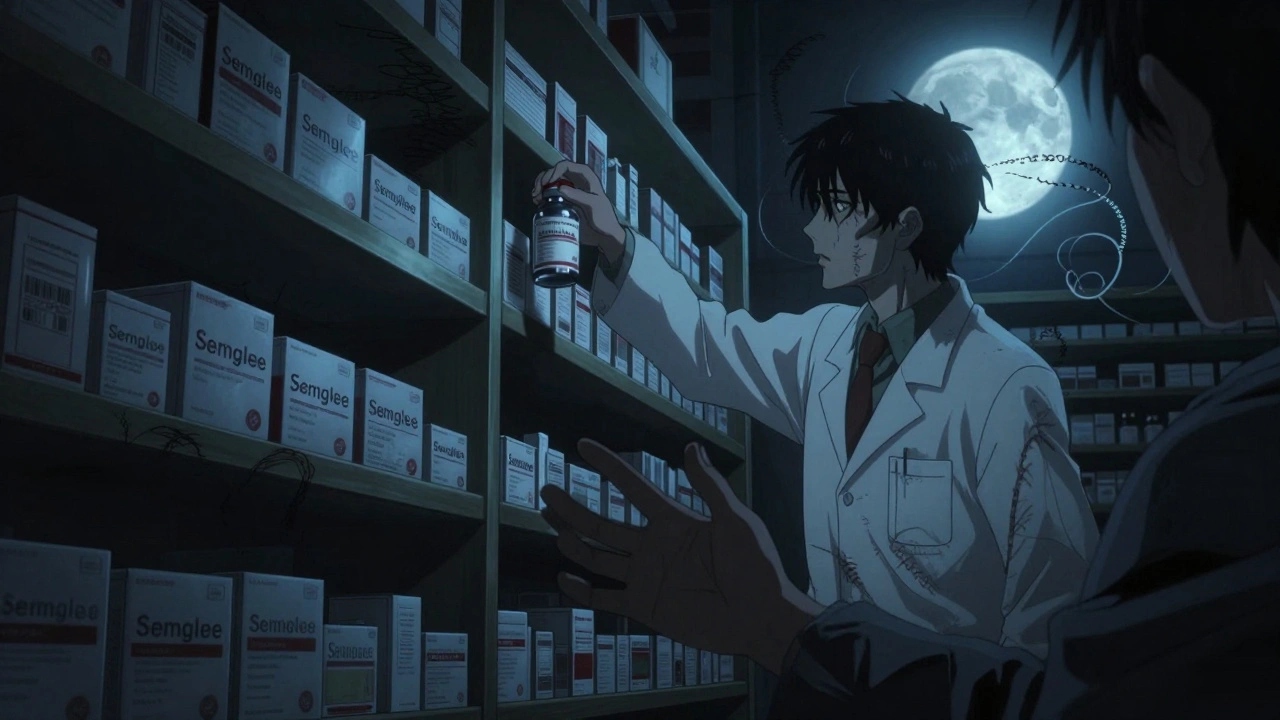
An interchangeable biosimilar isn’t just any biosimilar. It’s a special category created by the U.S. Food and Drug Administration (FDA) under the Biologics Price Competition and Innovation Act (BPCIA) of 2009. This designation allows pharmacists to swap out the original biologic drug-like Humira or Lantus-with a biosimilar version without needing to check back with the prescriber. It’s automatic. Just like how generic pills replace brand-name drugs under the Hatch-Waxman Act. But here’s the catch: not all biosimilars are interchangeable. In fact, as of November 2023, out of 41 FDA-approved biosimilars, only 10 have earned this status. The first was Semglee, an insulin glargine biosimilar approved in July 2021. The first interchangeable monoclonal antibody was Cyltezo, approved in August 2023, which can replace Humira without a doctor’s order. Interchangeability doesn’t mean the biosimilar is better. It just means the FDA has confirmed that switching back and forth between the reference product and the biosimilar won’t increase safety risks or reduce effectiveness. That’s a much higher bar than standard biosimilarity, which only requires proof that the biosimilar is highly similar to the original.Why Is Interchangeability So Hard to Get?
Unlike generic drugs, which are chemically identical copies of small-molecule medications, biosimilars are made from living cells. Think of them like handmade replicas of a complex sculpture-no two are exactly alike. That’s why the FDA demands extra proof before allowing automatic substitution. To qualify as interchangeable, a manufacturer must run switching studies. These involve giving patients multiple rounds of the reference drug and the biosimilar, switching between them at least twice. Researchers then track whether this back-and-forth causes any unexpected side effects, changes in immune response, or drops in effectiveness. The data must show no clinically meaningful differences after these switches. The FDA’s guidance, updated in January 2023, requires statistical proof that the biosimilar performs just as reliably as the original-even after multiple switches. This isn’t just about matching one dose. It’s about proving consistency over time, across different patients, in different conditions. Compare that to the European Union, where no formal interchangeability designation exists. In Europe, substitution decisions are left to doctors or pharmacists, and there’s no requirement for switching studies. The U.S. is the only country with this specific legal pathway.State Laws Are a Mess
Even if the FDA says a biosimilar is interchangeable, that doesn’t mean it can be automatically swapped everywhere. Each state has its own rules. Forty states, including Arizona and California, allow pharmacists to substitute interchangeable biosimilars without contacting the prescriber. But even in those states, there are hoops to jump through. In Arizona, pharmacists must notify the patient, record the exact product and manufacturer, send a notice to the doctor within five business days, and keep records for seven years. Six states and Washington D.C. only allow substitution if it saves the patient money. Four states-Alabama, Indiana, South Carolina, and Washington-require the prescriber’s explicit approval before any substitution can happen. And in some places, pharmacists have to check whether the patient’s insurance plan mandates substitution. This patchwork creates real confusion. A 2022 survey by the National Community Pharmacists Association found that 67% of independent pharmacists struggled to keep up with state-specific rules. One pharmacist on Reddit wrote: “In California, I have to check if it’s lower cost, but in Arizona I don’t. My pharmacy system doesn’t differentiate between states.”
Interchangeable vs. Non-Interchangeable: What’s the Real Difference?
Let’s be clear: every FDA-approved biosimilar-interchangeable or not-is safe and effective. The FDA insists that all biosimilars meet the same high standards for quality, purity, and potency as the original biologic. The only difference is who gets to decide when to switch: the doctor, or the pharmacist. Non-interchangeable biosimilars still offer big cost savings-typically 15% to 30% less than the reference product, according to a 2022 RAND Corporation study. But they can’t be swapped automatically. That means if your doctor prescribes Humira, you’ll get Humira, unless you or your doctor specifically asks for a biosimilar. Interchangeable biosimilars, on the other hand, can be substituted without any action from the prescriber. That’s why they’re driving faster adoption. In the insulin market, Semglee captured 17.3% of the market within six months of launch. Non-interchangeable biosimilars took much longer to reach similar levels.What Do Patients Really Think?
Patient experiences vary. Some are thrilled with the savings. One person on the Psoriasis Foundation forum wrote: “My dermatologist switched me from Humira to Hyrimoz. I saved $800 a month with no change in effectiveness.” Others aren’t so happy. Another patient reported an adverse reaction after their pharmacy automatically substituted Hadlima for Humira without telling them. Turns out, they were allergic to an excipient-a non-active ingredient-in the biosimilar. A 2022 survey by the National Psoriasis Foundation found that 63% of patients were satisfied after switching to a biosimilar. But 28% were upset they weren’t notified. That’s a big issue. Patients have a right to know what they’re taking, especially when it’s a complex biologic. And then there’s the concern about treatment persistence. Dr. Kevin Winthrop, a professor at Oregon Health & Science University, pointed to a study showing psoriasis patients switched to biosimilars were 20.3% more likely to stop treatment altogether. Could it be side effects? Lack of communication? Or just the psychological impact of being switched without consent?
What’s Next for Interchangeable Biosimilars?
The market is growing fast. By 2026, biosimilars could capture nearly half of the $168 billion global biologics market, according to Evaluate Pharma. But regulatory uncertainty is slowing things down. There’s a bill in Congress-the Biosimilar Red Tape Elimination Act (H.R. 9500)-that wants to scrap the switching study requirement. Proponents, including the Biosimilars Council, argue it would speed up access and lower prices. Opponents, like PhRMA, warn it could compromise safety. Meanwhile, the FDA is working on streamlining its guidance. A 2023 draft proposal suggests reducing the burden of switching studies, possibly allowing data from one product to support interchangeability for others in the same class. Pharmacists are getting better trained. The American Pharmacists Association has certified over 12,450 pharmacists in biosimilars as of October 2023. But the learning curve is steep. Pharmacists now spend an average of 8.7 hours a year just keeping up with changing laws.What Should You Do as a Patient?
If you’re on a biologic drug, here’s what you need to know:- Ask your doctor if a biosimilar is an option-and whether it’s interchangeable.
- Check your prescription. If your doctor writes “dispense as written” or uses a DAW code like “DAW 1,” substitution is blocked.
- Always ask your pharmacist: “Is this the same drug my doctor prescribed?”
- If you’re switched without warning, call your doctor. Report any new side effects.
- Know your state’s laws. If you live in Alabama or Washington, your pharmacist can’t substitute without your doctor’s OK.
Final Thoughts
Interchangeability is a powerful tool. It’s designed to lower costs and expand access to biologics that can cost over $20,000 a year. But it’s not a simple swap. It’s a complex system built on science, law, and patient rights. The U.S. has created a unique path-one that no other country follows. And while it’s working for some, it’s confusing for others. The goal should be clear: safe, affordable access to biologics, with transparency and choice at the center. The next few years will decide whether interchangeability becomes a cornerstone of American healthcare-or a regulatory headache that holds back progress.Can a pharmacist substitute any biosimilar for my biologic drug?
No. Only biosimilars that have received FDA interchangeability designation can be automatically substituted. As of late 2023, only 10 out of 41 approved biosimilars have this status. Even then, state laws may restrict substitution. Always check with your pharmacist and review your prescription for "dispense as written" instructions.
Are interchangeable biosimilars safer than non-interchangeable ones?
No. All FDA-approved biosimilars-interchangeable or not-are held to the same safety and effectiveness standards. The interchangeability designation only means the FDA has confirmed that switching between the reference product and the biosimilar multiple times won’t cause harm. It does not mean the interchangeable version is better or more effective.
Why don’t other countries have interchangeable biosimilars?
The U.S. is the only country with a formal regulatory pathway for automatic pharmacy-level substitution. The European Union, Canada, and Japan all approve biosimilars but leave substitution decisions to prescribers or require additional clinical data without using the term "interchangeable." The U.S. system was designed to drive competition and lower prices through automatic substitution, which other countries have chosen not to adopt.
Can I be switched to a different biosimilar without my doctor’s approval?
No. Interchangeability only applies to substitution with the original reference product, not between different biosimilars. For example, if you’re on Humira, you can be switched to Cyltezo (an interchangeable biosimilar) without a new prescription. But if your pharmacist tries to switch you from Cyltezo to another biosimilar like Hyrimoz, they need your doctor’s permission-even if both are interchangeable.
How do I know if I’ve been switched to a biosimilar?
Your pharmacy is required to notify you in many states, but not all. Always check the label on your medication box-it must list the manufacturer and product name. If you see a name you don’t recognize (like Hyrimoz, Semglee, or Cyltezo), ask your pharmacist. You can also check your insurance explanation of benefits (EOB) or contact your prescriber to confirm what was dispensed.

Let me break this down real simple-interchangeability isn’t about safety, it’s about economics. The FDA’s bar is high because biosimilars are biological nightmares to replicate. Unlike generics, you can’t just mix chemicals in a beaker. You’re dealing with living cells, protein folding, glycosylation patterns-this ain’t aspirin. The switching studies? Necessary. The state laws? A fucking mess. One state says notify the doc, another says only if cheaper, another says no substitution at all. Pharmacies are drowning in paperwork while patients get confused. We need federal standardization, not 50 different rulebooks.
So let me get this straight-you’re telling me my insurance company can swap my Humira for some random biosimilar without even asking me? And I’m supposed to be grateful because it’s ‘cheaper’? I had a reaction to Hadlima. Not the drug itself-some filler they used. My skin broke out like I’d been dipped in acid. No one told me I’d been switched. No one asked. And now my dermatologist says ‘it’s fine, it’s FDA-approved.’ Fine? Fine?! I didn’t sign up for a science experiment. This isn’t progress, it’s negligence wrapped in a corporate buzzword.
I’ve been on a biosimilar for my RA for over a year now-Cyltezo after Humira. No issues. No flare-ups. Saved me $700/month. I get why people are nervous-it’s a big change. But the science is solid. I read the FDA’s guidance. The switching studies are brutal, honestly. They make you go back and forth between drugs like a lab rat. If it passed that? It’s good. I wish pharmacists would just text me when they switch me, though. A quick ‘Hey, you got Cyltezo today’ would go a long way. Just a little respect for the patient.
interchangeable biosimilars are just generics with a fancy title. the system is broken. states are chaotic. patients are confused. doctors are overwhelmed. pharmacists are tired. save money yes but dont pretend its magic.
Y’all need to chillllll 😌 I switched to Semglee and my insulin costs dropped from $1,200 to $180. Like… what’s the problem? 🙃 I know people are scared of change but this isn’t a horror movie. The FDA didn’t just slap a sticker on it-they ran 10+ clinical trials. And if you’re worried? Just say NO. You have rights. Ask for the original. Write "dispense as written" on your script. 💪 You got this! #BiosimilarWin #SaveYourWallet
The entire interchangeable biosimilar framework is a regulatory farce designed to appease insurance CEOs. The FDA’s switching studies are statistically underpowered and based on cherry-picked patient populations. Real-world data shows higher discontinuation rates. And don’t get me started on state laws-this isn’t healthcare policy, it’s a bureaucratic parody. The EU gets it right: leave substitution to clinicians who know the patient. Not a pharmacist who’s trying to hit a cost-saving quota. This isn’t innovation. It’s cost-shifting disguised as progress.
As someone who’s worked in rural clinics across three states, I’ve seen this play out. In Alabama, we can’t swap without a doc’s note-good. In California, it’s automatic unless the patient objects-also good. But the real issue? Communication. I’ve had patients show up confused because their label says "Hyrimoz" but their old script said "Humira." We need a universal patient notification system-like a QR code on the bottle that links to a simple explainer video in 5 languages. Not a 10-page pamphlet. Just: "This is not your usual drug. Here’s why it’s safe. Here’s what to watch for." Simple. Clear. Human.
in Nigeria we don't even have biosimilars properly regulated yet. here if you get a drug, you pray it works. i read this and i'm like wow america has so many rules for saving money. we just hope the medicine doesn't kill us. you guys have it complicated but also lucky. we don't even know if the bottle has the right stuff inside.
Okay but why are we even talking about this like it's a big deal? I got switched to Cyltezo and I didn't even notice. My skin didn't explode. I didn't die. My bank account didn't cry. Why is everyone acting like this is some kind of medical betrayal? You think your Humira is magic? Nah. It's just a protein. They made a copy. It works. Get over it. Also stop complaining about state laws-your pharmacy system should auto-detect your location. If it doesn't, fire them. This is 2024, not 1999.
Interchangeable? More like interchangeable-without-consent. And the FDA? They’re just rubber-stamping this because Big Pharma wants to kill the biologics market. Patients are being treated like lab rats. And now pharmacists are playing doctor? This is dangerous. And the fact that you can’t switch between biosimilars? That’s just adding confusion on top of incompetence. Someone’s going to get hurt. Mark my words.