Biosimilars: What They Are, How They Compare to Biologics, and Why They Matter
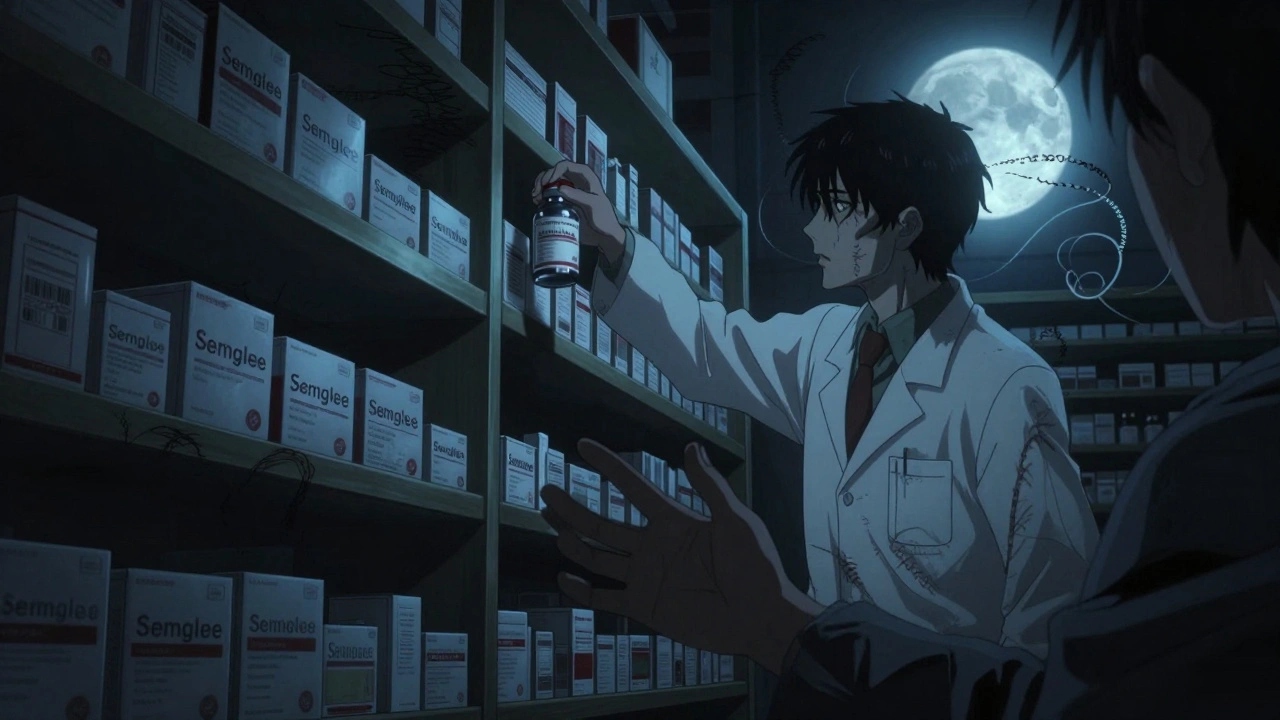
When you hear biosimilars, highly similar versions of complex biologic drugs that are not exact copies but meet strict regulatory standards for safety and effectiveness. Also known as biologic generics, they are designed to work just like the original biologic medicine—whether it’s for rheumatoid arthritis, cancer, or autoimmune conditions—but at a fraction of the cost. Unlike traditional generics, which are chemically identical to their brand-name counterparts, biosimilars are made from living cells. That means they’re more like a close cousin than a twin. The FDA and European Medicines Agency require them to show no meaningful difference in safety, purity, or potency compared to the original biologic drug.
Biologic drugs themselves are made from proteins, antibodies, or other biological materials, often targeting specific parts of the immune system. Drugs like Humira, Enbrel, and Remicade are biologics used to treat conditions like Crohn’s disease or psoriasis. Because they’re so complex, copying them exactly isn’t possible. That’s where biosimilars, medications developed to match the clinical performance of a reference biologic drug. Also known as follow-on biologics, they undergo rigorous testing to prove they produce the same results in patients. This isn’t just theory—it’s practice. Studies show biosimilars for rheumatoid arthritis, like those based on adalimumab, work just as well as the brand name in real-world use. Patients see the same reduction in joint pain and inflammation, with no increase in side effects.
But biosimilars aren’t just about cost—they’re about access. Many people can’t afford biologics, which can run over $20,000 a year. Biosimilars often cost 15% to 30% less, and in some cases even more. That difference can mean the difference between starting treatment and delaying it. And while some doctors and patients still hesitate, that’s often because of confusion, not science. The FDA doesn’t approve a biosimilar unless it’s proven to be as safe and effective. In fact, millions of doses have been given worldwide with no safety red flags.
What you won’t find in this collection are claims that biosimilars are "inferior" or "experimental." Instead, you’ll see real discussions about how they’re regulated, how pharmacists verify them, and how switching from a brand biologic to a biosimilar works in practice. You’ll also find posts that explain how these drugs fit into the bigger picture of generic prescribing, therapeutic equivalence, and drug pricing trends. If you’ve ever wondered why your doctor suggested a biosimilar, or if you’re worried about switching from a brand-name biologic, this is the place to get clear, no-fluff answers.
When Can Biosimilars Be Automatically Substituted? Understanding Interchangeability in the U.S.
Interchangeable biosimilars can be automatically swapped for brand-name biologics at the pharmacy level in the U.S., but only under strict FDA rules and varying state laws. Learn how they work, who can substitute them, and what patients need to know.
read more