Biosimilar Substitution: What It Means for Your Medication Choices
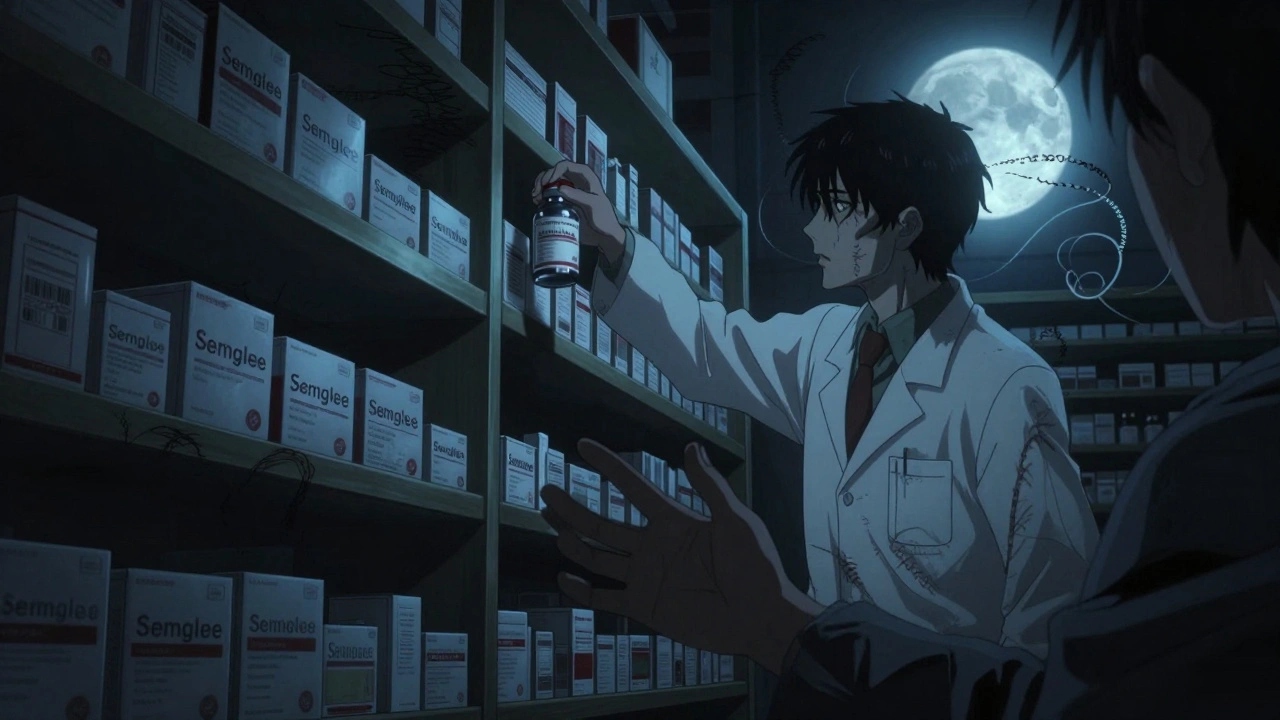
When you hear biosimilar substitution, the process of replacing a brand-name biologic drug with a closely similar version approved by health regulators. Also known as biologic switching, it’s not just another way to cut costs—it’s a shift in how millions get treated for conditions like rheumatoid arthritis, Crohn’s disease, and cancer. Unlike traditional generics, which copy small-molecule drugs, biosimilars are made from living cells. That means they’re more complex, harder to replicate exactly, and require stricter testing to prove they work the same way in your body.
That’s why therapeutic equivalence, the standard that proves a drug performs the same way as the original in real patients matters so much. The FDA and other global agencies don’t just look at chemical makeup—they check how the drug behaves in your bloodstream, how long it lasts, and whether it causes the same side effects. If a biosimilar passes all these tests, it’s considered interchangeable in many cases. But here’s the catch: not all biosimilars are approved for automatic substitution. Some require a doctor’s explicit OK. And that’s where confusion starts. Many patients worry switching will make their treatment less effective. But studies from the CDC and European Medicines Agency show that when properly monitored, biosimilar substitution doesn’t increase risks of flare-ups or side effects.
It’s also not just about price. While biosimilars can be 20% to 40% cheaper than the original biologic, the real win is access. Before biosimilars, drugs like Humira or Enbrel cost over $70,000 a year. Now, with competition, many patients get them for under $20,000. But cheaper doesn’t mean automatic. Pharmacists follow strict rules when swapping—often checking state laws, insurance rules, and whether the prescriber allowed substitution. Some insurers push biosimilars hard. Others don’t. And if you’re on biologic drugs, complex medications made from living organisms used to treat autoimmune and chronic diseases for years, switching can feel scary. That’s normal. But the data is clear: for most people, it’s safe.
You’ll find posts here that dig into the real-world side of this. Like how generic drug switching works for warfarin—where tiny changes can throw off your INR levels. Or how pharmacists use the FDA’s Orange Book to confirm equivalence. You’ll see why some patients stick with brand-name drugs even when it costs more, and how doctors are adapting to new prescribing rules in 2025. There’s also a deep look at foreign manufacturing, FDA inspections, and what happens when a biosimilar’s inactive ingredients don’t match the original. These aren’t theoretical debates. They’re daily decisions that affect your health, your wallet, and your peace of mind.
Whether you’re on a biologic now, considering a switch, or just trying to understand your prescription label, this collection gives you the facts—not the marketing. No fluff. No jargon. Just what you need to know to ask the right questions and make confident choices.
When Can Biosimilars Be Automatically Substituted? Understanding Interchangeability in the U.S.
Interchangeable biosimilars can be automatically swapped for brand-name biologics at the pharmacy level in the U.S., but only under strict FDA rules and varying state laws. Learn how they work, who can substitute them, and what patients need to know.
read more