Anticholinergic Burden: What It Is and How It Affects Your Medications
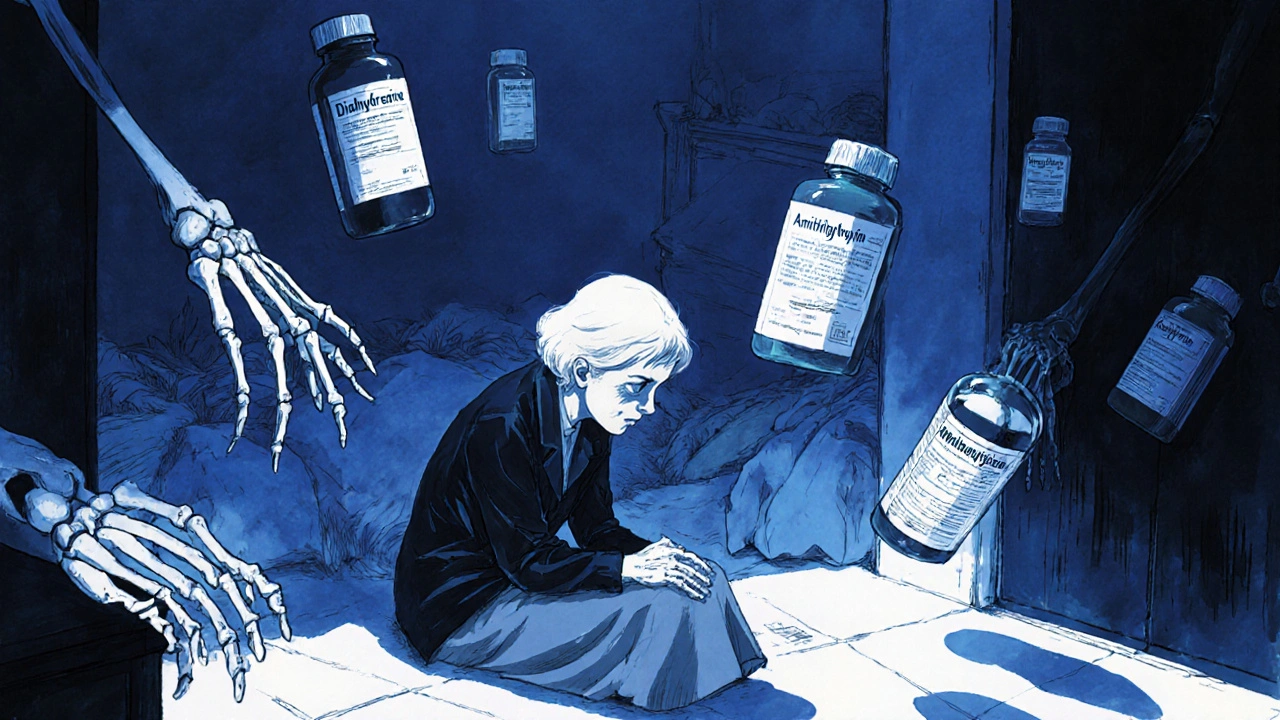
When you take more than one anticholinergic burden, the total effect of all medications in your system that block acetylcholine, a key brain chemical. Also known as anticholinergic load, it doesn’t show up on blood tests — but it can quietly weaken your memory, balance, and even your ability to think clearly over time. This isn’t about one bad pill. It’s about the slow accumulation of common drugs — from sleep aids and allergy pills to bladder meds and antidepressants — that all do the same thing: shut down acetylcholine signals in your brain and body.
Think of acetylcholine as the brain’s messenger for focus, memory, and muscle control. When too many drugs block it, your brain struggles to keep up. A 2019 study in JAMA Internal Medicine found people with high anticholinergic burden were 40% more likely to develop dementia over 10 years — even if they were young and otherwise healthy. And it’s not just older adults. People in their 40s and 50s taking multiple anticholinergics are at risk too. You might not feel it right away, but over months or years, the fog builds. Trouble remembering names. Forgetting where you put your keys. Feeling dizzy when you stand up. These aren’t just aging — they’re signs your meds might be working against you.
The real problem? Many of these drugs are sold over the counter. Doxylamine succinate, a common sleep aid and allergy medication with strong anticholinergic effects. Also known as Unisom, it’s in dozens of sleep and cold products. Same with dimenhydrinate, the active ingredient in Dramamine, used for motion sickness and sometimes allergies. Also known as Dramamine, it’s another silent contributor to the burden. Even some antidepressants like mirtazapine, a drug often prescribed for depression and sleep, known for its anticholinergic properties. Also known as Remeron, it’s one of the most likely to cause weight gain and mental fogginess. These aren’t rare or experimental drugs — they’re everyday prescriptions and OTC staples. And if you’re taking more than one, the effects add up fast.
What you can do isn’t about stopping meds cold. It’s about awareness. If you’re on three or more medications — even if they’re for different issues — ask your doctor or pharmacist: "Could any of these be adding to my anticholinergic burden?" There are often safer alternatives. For allergies, loratadine or cetirizine don’t block acetylcholine. For sleep, melatonin or behavioral changes might work better than doxylamine. For bladder control, newer options exist that don’t hit your brain as hard.
Below, you’ll find real-world guides that break down exactly which drugs contribute to this burden — and how to spot them on your prescription labels. You’ll see how liver disease changes how your body handles these drugs, how generic substitutions can sneak in higher-risk versions, and what to watch for when combining meds. This isn’t theory. It’s what people are already experiencing — and what you can change before it’s too late.
Cumulative Anticholinergic Burden: How Antihistamines Combine with Other Medications to Risk Cognitive Decline
Cumulative anticholinergic burden from antihistamines and other medications increases dementia and fall risks in older adults. Learn how to spot hidden drug interactions and switch to safer alternatives.
read more