Anticholinergic Burden Calculator
This tool calculates your cumulative anticholinergic burden score using the ACB Scale. Enter your medications to see your total score and potential risks.
Your Medications
Your Anticholinergic Burden Score
Every year, thousands of older adults in the UK and beyond start taking antihistamines for allergies or sleep-often without realizing they’re adding to a hidden danger. These common pills, like diphenhydramine (Benadryl) or chlorpheniramine, don’t just stop sneezing. They also block acetylcholine, a brain chemical vital for memory, focus, and muscle control. When taken alone, the risk might seem small. But when combined with other medications-like antidepressants, bladder pills, or sleep aids-their effects stack up. This buildup is called cumulative anticholinergic burden. And it’s one of the most underdiagnosed causes of memory loss, falls, and hospital stays in people over 65.
What Exactly Is Anticholinergic Burden?
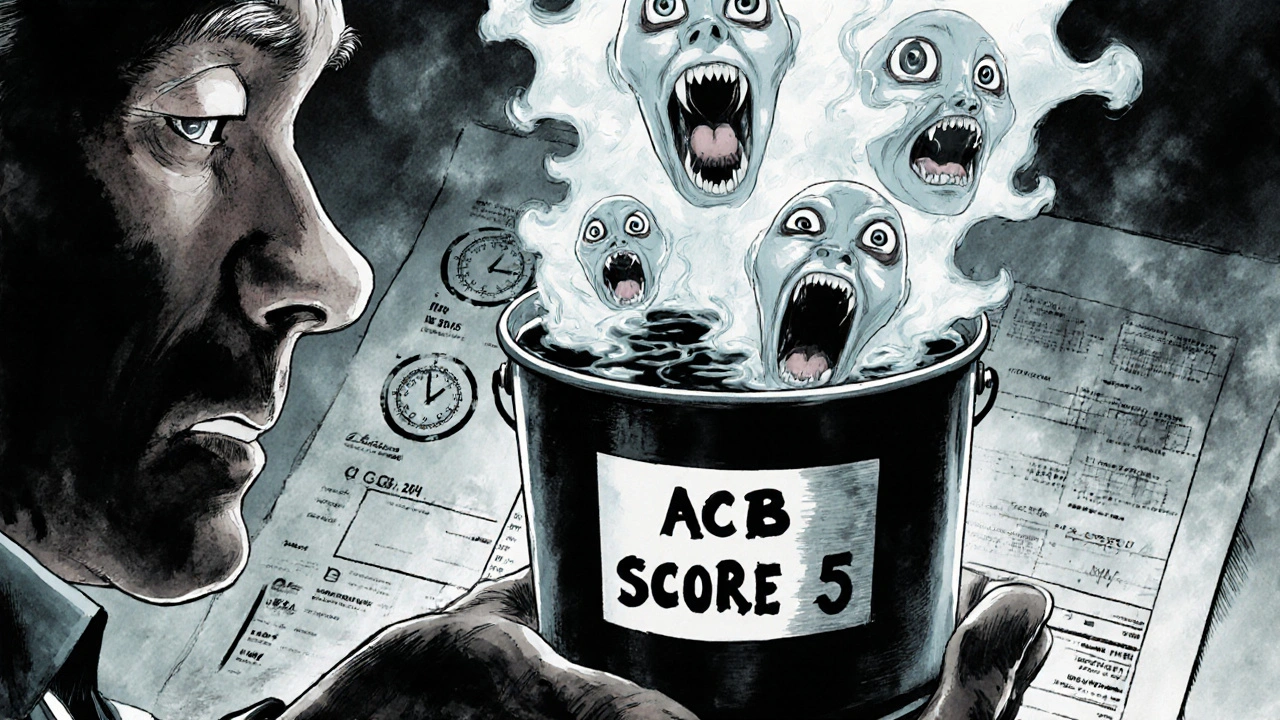
Anticholinergic burden isn’t about one drug. It’s about the total effect of all the drugs you take that interfere with acetylcholine. Think of it like filling a bucket. Each medication adds a cup of water. Some cups are small-others are full. Over time, the bucket overflows. That’s when symptoms appear: confusion, dry mouth, constipation, trouble urinating, blurred vision, or sudden memory lapses. These aren’t just side effects. They’re warning signs.The ACB Scale (Anticholinergic Burden Scale) is the tool doctors use to measure this. It rates every medication on a scale from 0 to 3:
- Score 0: No anticholinergic effect (like loratadine or cetirizine)
- Score 1: Mild effect (some diuretics, low-dose antidepressants)
- Score 2-3: Strong effect (diphenhydramine, amitriptyline, oxybutynin, benztropine)
Here’s the catch: if your total score hits 3 or higher, your risk of dementia, falls, and hospitalization jumps dramatically. A 2015 study in JAMA Internal Medicine followed over 3,400 people for seven years. Those who took strong anticholinergics daily for more than three years had a 54% higher chance of developing dementia. And nearly a third of those strong medications? Antihistamines.
Why Antihistamines Are a Silent Problem
First-generation antihistamines-like diphenhydramine, chlorpheniramine, and promethazine-are the worst offenders. They cross the blood-brain barrier easily and hit acetylcholine receptors hard. That’s why they make you drowsy. But that same trait makes them dangerous over time.People don’t realize these are anticholinergic drugs. They buy them over the counter for allergies, colds, or sleep. A 70-year-old might take one for hay fever in the morning, another at night to help them sleep. Meanwhile, their doctor prescribed amitriptyline for nerve pain and oxybutynin for an overactive bladder. Each drug on its own might seem fine. Together? That’s an ACB score of 4 or 5.
That’s not rare. The American Geriatrics Society says half of all older adults take five or more medications daily. And 20-50% of them are exposed to at least one strong anticholinergic. Antihistamines alone make up 15-25% of that exposure. The FDA added warnings to these labels in 2017. The European Medicines Agency followed in 2019. But most patients still don’t know.
How These Drugs Work Together
It’s not just antihistamines. They’re often part of a dangerous cocktail:- Tricyclic antidepressants (amitriptyline, nortriptyline): Used for depression, nerve pain, migraines. ACB score: 3.
- Bladder medications (oxybutynin, tolterodine): For overactive bladder. ACB score: 2-3.
- Parkinson’s drugs (benztropine, trihexyphenidyl): Used to control tremors. ACB score: 2-3.
- Sleep aids (doxepin, doxylamine): Often taken nightly. ACB score: 2-3.
- Stomach meds (hyoscine, prochlorperazine): For nausea or motion sickness. ACB score: 1-2.
Combine even one of these with a daily antihistamine, and you’re likely over the danger line. A 2021 case study from NPS MedicineWise showed a 72-year-old woman with an ACB score of 5. She was misdiagnosed with dementia. After stopping diphenhydramine and switching to a non-anticholinergic sleep aid, her memory improved, and her falls dropped by 75% in six months.
What Symptoms Should You Watch For?
These aren’t normal signs of aging. If someone you care about suddenly:- Forgets where they put their keys-or what day it is
- Stumbles more often or gets up slowly from a chair
- Complains of dry mouth, constipation, or trouble peeing
- Seems confused after starting a new medication
That’s not just getting older. That’s anticholinergic burden. The Hull University Teaching Hospitals report that 15-20% of older adults on multiple anticholinergics experience confusion. And it’s reversible-if caught early.
One Reddit user shared that their 78-year-old mother was diagnosed with early dementia. She was taking diphenhydramine nightly and amitriptyline daily. Her ACB score was 4. After stopping the Benadryl, her memory returned within weeks. The doctor had never asked about over-the-counter meds.
How to Check and Reduce Your Burden
You don’t need a PhD to take action. Here’s how:- Make a full list of everything you take-prescription, over-the-counter, supplements, herbal remedies. Include doses and how often.
- Use the ACB Scale (freely available online). Match each drug to its score. Add them up.
- Look for red flags: Any drug with a score of 2 or 3? That’s a warning sign.
- Ask your pharmacist or GP: ‘Could any of these be adding up to cause memory or balance problems?’
Switching to second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), or fexofenadine (Allegra) cuts the burden to nearly zero. They work just as well for allergies-with no drowsiness or brain fog.
For sleep? Try melatonin instead of diphenhydramine. For bladder issues? Consider pelvic floor exercises or newer non-anticholinergic options like mirabegron. For depression? SSRIs like sertraline have no anticholinergic effect.
Deprescribing doesn’t mean stopping cold turkey. Work with your doctor to taper off slowly. The IU Center for Aging Research found that 65% of patients successfully switch within 4-8 weeks when given a plan.
Why This Matters More Than You Think
This isn’t just about memory. It’s about independence. Falls lead to fractures. Fractures lead to hospital stays. Hospital stays lead to long-term care. And all of it can be linked to medication buildup.Research from Campbell et al. (2016) shows that strong anticholinergics increase hospital admissions by 33% in a year. Mild ones still raise them by 11%. Reducing this burden cuts healthcare costs by 11-33% annually. In the UK, NHS England estimates that tackling antihistamine-related anticholinergic burden could save £217 million a year in hospital admissions alone.
And it’s getting worse. The American Geriatrics Society updated its Beers Criteria in 2023 to say: ‘Chronic use of first-generation antihistamines should be avoided in older adults due to strong evidence of cognitive impairment even at low cumulative doses.’ That’s not a suggestion. It’s a red flag.
Meanwhile, hospitals are waking up. By 2023, 62% of primary care practices in the US started using ACB screening tools. CMS now ties Medicare Star Ratings to how well clinics reduce anticholinergic burden. In Bristol, some GP practices are now training staff to ask every patient over 65: ‘Are you taking any sleep or allergy pills regularly?’
What You Can Do Today
If you or someone you love is over 65 and taking antihistamines-even just a few times a week-here’s your next step:- Check your medicine cabinet. Look for diphenhydramine, chlorpheniramine, promethazine, or doxylamine.
- Ask your pharmacist to run a free anticholinergic burden check. Most will do it without an appointment.
- Bring your full list of meds to your next doctor visit. Say: ‘I’m worried these might be affecting my memory or balance.’
- Replace first-gen antihistamines with second-gen ones. They’re just as effective and much safer.
You don’t need to be a medical expert to save someone’s brain. You just need to ask the right question.
Can antihistamines cause dementia?
Yes-when taken long-term and especially when combined with other anticholinergic drugs. A 2015 JAMA study found that people who took strong anticholinergics daily for more than three years had a 54% higher risk of dementia. Antihistamines like diphenhydramine made up nearly a third of those drugs in the study. The risk isn’t from occasional use-it’s from daily, long-term exposure.
Are all antihistamines dangerous for older adults?
No. Only first-generation antihistamines-like diphenhydramine, chlorpheniramine, and promethazine-are strongly anticholinergic. Second-generation ones like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) have little to no effect on the brain and are much safer for long-term use in older adults.
How do I know if I’m taking too many anticholinergic drugs?
Use the ACB Scale to score each medication. Add up the numbers. If your total is 3 or higher, you’re at increased risk for cognitive decline, falls, and hospitalization. Common culprits include sleep aids, bladder meds, antidepressants, and over-the-counter allergy pills. Talk to your pharmacist or GP for a free review.
Can stopping antihistamines improve memory?
Yes-often quickly. In multiple case studies, older adults who stopped nightly diphenhydramine or similar drugs saw noticeable improvement in memory and alertness within weeks. One woman’s confusion cleared up after she stopped taking Benadryl with her antidepressant. Her ACB score dropped from 4 to 1. Her doctor had never asked about her over-the-counter meds.
Is it safe to stop antihistamines suddenly?
It depends. If you’ve been taking them daily for sleep or allergies, stopping suddenly might cause rebound symptoms like worse allergies or insomnia. Work with your doctor to taper off slowly and replace them with safer alternatives like melatonin for sleep or second-gen antihistamines for allergies. Most people transition successfully within 4-8 weeks.
What Comes Next?
The tide is turning. By 2027, 80% of healthcare systems in the US and UK are expected to screen patients over 65 for anticholinergic burden. EHR systems will soon auto-flag high-risk combinations. But until then, the burden is on you.Don’t wait for a fall, a hospital stay, or a dementia diagnosis. Look at your medicine cabinet today. Ask the question. Make the swap. Your brain-and your independence-depend on it.

I just found out my mom’s been taking Benadryl every night for 12 years… for SLEEP!!! I’m crying. I thought she was just aging. She’s been forgetting where she put her glasses, stumbling in the hallway, and now I realize it’s not dementia-it’s DOSE after DOSE of brain-rotting chemicals!!! I’m taking her to the pharmacist tomorrow. She’s switching to melatonin. I’m so mad at myself for not asking sooner!!!
this is all fearmongering. my grandma took benadryl for 40 years and lived to 98. you people are so scared of medicine youd rather take herbal tea and pray. stop overmedicating your brains with anxiety.
As someone who works with elderly patients in India, I see this every day. Grandparents take antihistamines for colds, then get prescribed amitriptyline for pain, then diphenhydramine again for sleep. No one connects the dots. The real tragedy? They’re not even told these are anticholinergic. We need community pharmacists to do simple ACB checks-like a blood pressure screen. It’s cheap, fast, and saves lives. No PhD needed. Just awareness.
It’s funny how we treat aging like a disease to be fixed with pills. We’re so quick to add, but never to subtract. The body isn’t a machine you keep tuning with more parts-it’s a garden. Sometimes, the healthiest thing you can do is pull the weeds. Anticholinergics? Those are the weeds. Second-gen antihistamines? That’s the compost. You don’t need a new drug to feel better-you just need to stop poisoning yourself with the old ones. And yes, your brain remembers that.
I’m not a doctor but I’m a daughter. My dad was misdiagnosed with mild cognitive impairment. He was on 4 meds with ACB score of 5. We stopped the Benadryl and the oxybutynin. Within 3 weeks-he was making jokes again. He remembered my dog’s name. He started gardening. It wasn’t dementia. It was a drug hangover. Please, if you’re over 65 and taking something for sleep or allergies-ask your pharmacist. Not your doctor. Your pharmacist. They know the math.
lol so benadryl is bad now? i thought it was just a sleepy pill. also why is everyone so obsessed with acb scale like its some secret cult code? i just want to sleep and not sneeze. also typo: 'diphenhydramine' took me 3 tries to spell. 🤦♀️
The evidence is robust, the guidelines are clear, and the cost of inaction is catastrophic. A systematic review of 12 cohort studies confirms a dose-dependent relationship between cumulative anticholinergic exposure and incident dementia. Immediate clinical action is warranted.
You’re not alone in feeling overwhelmed. If you’re reading this and thinking, ‘I didn’t know,’ that’s okay. The system didn’t tell you. But now you know. And that’s the first step. Start small-write down every pill in your cabinet. Talk to your pharmacist. Swap one thing. Maybe just replace the nighttime Benadryl with melatonin. That’s one less cup in the bucket. And that’s victory. You’re not failing-you’re learning. And that’s everything.