
For many people living with PTSD, the worst part isn’t the memories-it’s what happens when they close their eyes. Nightmares don’t just disturb sleep; they sabotage recovery. You wake up drenched in sweat, heart pounding, convinced you’re back in the moment that changed everything. And then the cycle starts again: fear of sleep, exhaustion, irritability, and a brain too wired to relax. It’s not laziness. It’s not weakness. It’s your nervous system stuck in fight-or-flight mode, even when you’re asleep.
Why PTSD Nightmares Are Different
Not all bad dreams are the same. PTSD nightmares aren’t just scary. They’re replayed. Exact. Unchanged. You’re back in the accident, the combat zone, the assault. These aren’t symbolic dreams. They’re neurological echoes. Research shows 71% to 90% of military veterans with PTSD experience them. Among civilians who’ve survived trauma, it’s still over half. That’s not rare. It’s the rule, not the exception. These nightmares aren’t caused by stress alone. They’re tied to how trauma rewires the brain’s fear circuits. The amygdala, your brain’s alarm system, stays on high alert. Meanwhile, the prefrontal cortex-the part that helps you calm down-gets quieter. Sleep, especially REM sleep, becomes a battleground. That’s when the brain tries to process emotions. But with PTSD, it doesn’t process. It replays.Prazosin: The Blood Pressure Drug That Changed Sleep for PTSD Patients
Prazosin wasn’t meant for nightmares. It was developed in 1976 to lower blood pressure. But in 2003, a VA doctor named Murray Raskind noticed something strange: veterans taking prazosin for hypertension were sleeping better. Their nightmares faded. He tested it. The results were clear. Prazosin blocks norepinephrine, a stress chemical that spikes during REM sleep in PTSD. Less norepinephrine = less fear flooding the brain at night. Today, it’s used off-label for PTSD nightmares. Most people start at 1 mg at bedtime. The dose slowly increases-usually by 1 mg each week-until it works or side effects appear. Typical doses range from 3 mg to 15 mg. Some need up to 25 mg. It’s not a magic pill. But for many, it’s the first time in years they’ve slept through the night without waking up screaming. But here’s the catch: prazosin doesn’t fix PTSD. It just quiets the nightmares. Studies show it reduces nightmare frequency by about 50% on average. But it doesn’t touch the underlying trauma. And it’s not without risks. Dizziness, low blood pressure, and nasal congestion are common. About 44% of users report side effects. Worse, 28% experience rebound nightmares when they stop taking it. That’s why doctors don’t recommend quitting cold turkey. Tapering matters. And despite years of use, the FDA hasn’t approved prazosin for nightmares. Why? Because some large trials-like the one funded by the Department of Defense in 2018-showed mixed results. Critics say the doses were too low. Others say the trials included people who didn’t even have frequent nightmares. The debate is still alive. But for many patients, the relief is real.CBT-I: The Therapy That Rewires Your Sleep
If prazosin is a quieting agent, CBT-I is a rebuild. Cognitive Behavioral Therapy for Insomnia isn’t about sleeping pills. It’s about changing the habits and thoughts that keep you awake. And for PTSD, it’s one of the most powerful tools we have. CBT-I usually takes 6 to 8 weekly sessions. Each is about an hour. You learn to:- Get out of bed if you’re awake for more than 20 minutes
- Limit time in bed to match how much you actually sleep (sleep restriction)
- Challenge thoughts like “I’ll never sleep again”
- Stop using your bed for anything but sleep and sex
- Practice relaxation techniques before bed
Imagery Rehearsal Therapy: Rewriting Your Nightmares
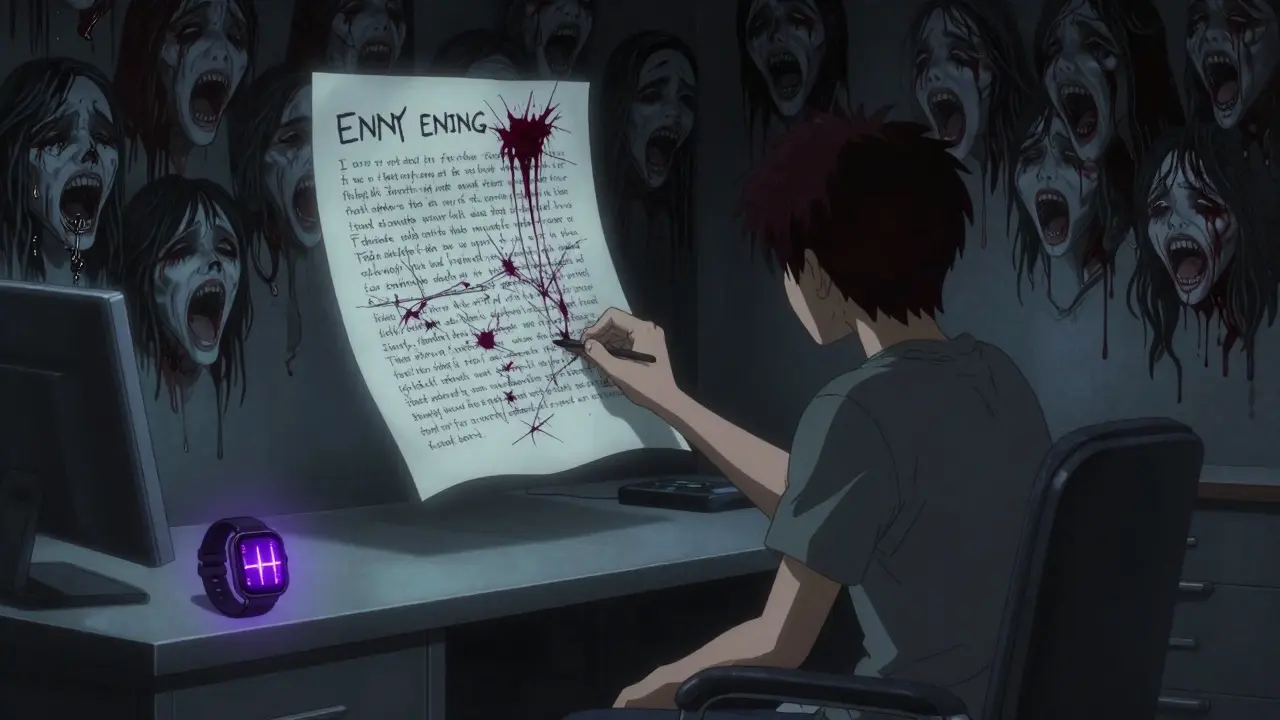
If CBT-I fixes your sleep habits, Imagery Rehearsal Therapy (IRT) rewires your nightmares themselves. You don’t just wait for them to stop. You change them. Here’s how it works: You write down your worst nightmare in detail. Then, you rewrite it. Not just a little. You change the ending. Maybe you escape. Maybe you fight back. Maybe you call for help. You rewrite it into something empowering, safe, or even absurd. Then, you rehearse the new version in your head for 10 to 20 minutes every day. Studies show 67% to 90% of PTSD patients see a major drop in nightmare frequency after just 3 to 5 sessions. One woman, a survivor of sexual assault, rewrote her nightmare from being trapped in a burning house to walking out of it holding a flashlight. She said, “It didn’t erase the memory. But it took the power away.” IRT works because it interrupts the fear loop. When you rehearse a new ending, your brain starts to treat the nightmare as something you can control. It’s not just distraction. It’s cognitive restructuring-applied directly to dreams. And unlike prazosin, there are no side effects. No dizziness. No crashes. Just effort. And results.Combining Treatments: The Best of Both Worlds
The strongest evidence doesn’t come from using one treatment alone. It comes from combining them. A 2022 VA study looked at CBT-I paired with Prolonged Exposure (PE), a trauma-focused therapy. The results were dramatic:- Insomnia severity dropped by 12.4 points (vs. 4.2 with PE alone)
- Sleep efficiency jumped 15.3%
- Total sleep time increased by 78 minutes

Why Some People Don’t Get Help
You’d think with all this evidence, everyone would be getting treatment. But they’re not. Only 32% of veterans in VA care get evidence-based psychotherapy. Nearly 78% get medication. Why? Because therapy is harder. It requires time. It requires facing trauma. It requires trust. And many clinics don’t have trained providers. Only 412 clinicians in the U.S. are certified in CBT-I. In rural areas, access is 47% lower than in cities. Insurance is another barrier. Many plans cover only 6 sessions of CBT-I-even though 8 are proven to work. Prazosin? It’s cheap. Generic. Easy to prescribe. And then there’s stigma. “Just take a pill.” “Stop having nightmares.” “You’re overreacting.” Those messages keep people silent. But nightmares aren’t a choice. They’re a symptom. And they’re treatable.What Works Now-and What’s Coming
Right now, the best approach is personalized:- If nightmares are your main problem and you’re not ready for trauma therapy, try prazosin-starting low, going slow, with your doctor monitoring your blood pressure.
- If you want long-term change without meds, try CBT-I or IRT. Both require effort, but they build resilience.
- If you can handle both, combine them. Trauma-focused therapy + sleep therapy = better outcomes than either alone.
- If you’re tech-savvy and have an Apple Watch, ask about NightWare. It’s FDA-approved and covered by some VA plans.
What to Do Next
If you’re struggling with PTSD nightmares:- Track your nightmares for two weeks. Write down frequency, intensity, and time of waking.
- Ask your doctor about prazosin-but only if you’re okay with monitoring blood pressure and potential side effects.
- Ask for a referral to a sleep specialist trained in CBT-I or IRT. Use the Society of Behavioral Sleep Medicine’s directory to find one.
- If you’re a veteran, contact your VA’s mental health department. Ask about Sleep SMART or NightWare.
- Don’t wait for the “perfect” time. Start small. One change. One step. Sleep recovery isn’t linear. But it’s possible.
Does prazosin cure PTSD nightmares permanently?
No. Prazosin reduces nightmare frequency while you’re taking it, but it doesn’t address the root cause of PTSD. Many people experience rebound nightmares when they stop. It’s a management tool, not a cure. For lasting change, pairing it with therapy like CBT-I or IRT is more effective.
Can I take prazosin with other PTSD medications?
Yes, but only under medical supervision. Prazosin is often used alongside SSRIs like sertraline or paroxetine, which are FDA-approved for PTSD. But combining it with other blood pressure medications or sedatives can increase dizziness or low blood pressure. Always tell your doctor about every medication or supplement you’re taking.
How long does it take for CBT-I to work for PTSD nightmares?
Most people see improvement in sleep within 2 to 4 weeks. Nightmare frequency often drops after 4 to 6 sessions. But the full benefits-like reduced daytime anxiety and better emotional control-take longer, usually 8 to 12 weeks. Consistency matters more than speed. The skills you learn last long after therapy ends.
Is IRT effective for non-veterans with PTSD?
Yes. Studies show IRT works just as well for civilian trauma survivors-people who’ve experienced sexual assault, accidents, or domestic violence-as it does for veterans. The mechanism is the same: rewriting the nightmare script reduces fear conditioning. A 2020 National Center for PTSD survey found 85% of civilian users reported reduced nightmare distress after IRT.
Can I use the NightWare app without an Apple Watch?
No. NightWare requires an Apple Watch Series 3 or later to detect physiological changes during REM sleep. It’s currently the only FDA-approved digital therapeutic for PTSD nightmares and only works with Apple’s hardware. Other apps exist, but none have FDA clearance for this specific use.
What if I can’t afford CBT-I or don’t have a therapist nearby?
The VA offers free CBT-I to eligible veterans through its Sleep SMART program. For civilians, the CBT-I Coach app (free on iOS and Android) provides a structured, evidence-based program you can use at home. It includes sleep tracking, education, and guided exercises. While not a replacement for a therapist, it’s a proven first step. Many people improve significantly using it alone.

Prazosin saved my life. I was waking up screaming every night for five years straight-no sleep, no peace, just terror replaying like a broken tape. Started at 1 mg, went up to 8 mg over six weeks. Didn’t feel like a miracle at first, but then one night… I slept through. No sweat. No heart pounding. Just… quiet. I cried. Not because I was happy-because I forgot what quiet felt like.
It’s not a cure. I know that. But it’s the first tool that let me breathe again. And now I’m doing CBT-I on top of it. Together? It’s like finally turning off the alarm after years of being stuck in a fire drill.
lol prazosin? bro just meditate. i did it in goa. no pills needed. trauma is just bad vibes man.
It’s profoundly tragic, isn’t it?-that we’ve reduced the sacred, soul-rending aftermath of human suffering to a pharmacological Band-Aid, a chemical soporific slipped into the twilight of a broken nervous system… and yet, we call it progress? Prazosin-this antihypertensive relic from the 70s-is the closest thing we’ve got to a temporal escape hatch from the labyrinth of our own neurobiology… but it doesn’t heal the wound; it merely mutes the scream.
And CBT-I? A beautiful, almost poetic act of cognitive reclamation-forcing the mind, through ritual and restriction, to relearn the sanctuary of the bed… as if sleep were a language we’d forgotten how to speak. But tell me: when the body remembers trauma in its bones, can a behavioral protocol truly rewire the somatic echo? Or are we just teaching the ghost to be polite?
For anyone reading this and thinking, ‘I can’t do CBT-I because I’m too tired’-I get it. I was there. The first week of sleep restriction? I was a zombie. But here’s the thing: your brain doesn’t need perfection. It needs consistency. Even if you only do 10 minutes of imagery rehearsal before bed, or write down one nightmare and rewrite one line of it? That’s a win.
And if you’re on prazosin? Don’t quit cold turkey. I did. Rebound nightmares were worse than the original. Tapered over 6 weeks? No crashes. Just gradual quiet.
This isn’t about being strong. It’s about being stubborn enough to show up for yourself-even when you’re exhausted. You’ve survived the trauma. Now show up for the sleep.
I tried NightWare. It’s… weird. Like your watch is whispering, ‘Hey, you’re having a nightmare again. Chill.’ But it worked. First night, I woke up confused-like I’d been dreaming about a dragon, then suddenly I was just… awake. No sweat. No panic.
And I didn’t even realize how much I’d been dreading bedtime until I stopped dreading it. I used to check the time before I fell asleep like it was a countdown to disaster. Now? I just… close my eyes. And sometimes, I even smile.
It’s not magic. But it’s mine.
Prazosin works. CBT-I works. IRT works. Stop arguing and find a provider.
cmon guys prazosin is just a bandaid. real men face their demons. i did it in 3 weeks with breath work and a 5am run. no pills. no therapy. just willpower.
I’ve been a therapist for 18 years, and I’ve seen people heal in ways I never expected. But I’ve also seen too many fall through the cracks because the system doesn’t make therapy accessible. Prazosin is cheap. CBT-I requires time, training, and trust. And trust? That’s the hardest part to build.
I wish we treated sleep the way we treat physical injuries. You wouldn’t tell someone with a broken leg to ‘just walk it off.’ So why do we say that to someone whose brain won’t let them rest?
This post? It’s not just information. It’s a lifeline. Thank you for writing it.
How delightful. A 2022 VA study with statistically significant results… and yet, only 32% of veterans receive evidence-based therapy. How quaint. We’ve got the science. We’ve got the tools. We’ve got the funding. And yet, we still treat trauma like a personal failing rather than a public health crisis.
Let’s be clear: if this were a cancer, we’d have marches, celebrity endorsements, and congressional hearings. But PTSD nightmares? Oh, just take a pill. Or meditate. Or ‘be strong.’
How progressive of us.
i started cbt-i last month. week 2 was hell. i only slept 3 hrs a night. but today? i slept 7. no nightmare. no panic. just… peace. its not easy. but its worth it.
You guys are all missing the point. Nightmares aren’t neurological-they’re spiritual. Prazosin? That’s just chemical denial. CBT-I? That’s brainwashing yourself into ignoring the truth. The real fix? Shamanic journeying. I did a 7-day sweat lodge retreat in Sedona. My nightmares? They showed up, bowed, and left. No drugs. No apps. Just ancestral wisdom.
Look, I’m not saying your methods are wrong-I’m saying they’re incomplete. You’re treating symptoms while ignoring the soul’s scream. And the soul? It doesn’t care about FDA approvals.
Keith, I get that you’re trying to be profound. But for the 12-year-old kid who wakes up screaming because his dad died in a car crash, ‘ancestral wisdom’ doesn’t put food on the table or help him get to school.
Prazosin let him sleep. CBT-I let him trust his bed again. NightWare let him stop checking his heart rate every time he closed his eyes.
Spiritual? Maybe. But right now, science is the only thing keeping him alive.