
Every year, thousands of people in the UK and beyond suffer liver damage not from alcohol, viruses, or poor diet-but from medications they took as directed. It’s not rare. It’s not exotic. It’s medication-related liver damage, and it’s quietly becoming one of the leading causes of acute liver failure in Western countries. Many don’t realize it’s happening until it’s too late. The liver doesn’t scream. It whispers. And by the time you hear it, you might already be in crisis.
What Medication-Related Liver Damage Actually Looks Like
When we say "medication-related liver damage," we’re talking about drug-induced liver injury (DILI). It can come from prescription drugs, over-the-counter painkillers, herbal teas, or those "natural" supplements you buy online. It’s not always the drug’s fault-it’s often your body’s reaction to it. Some people develop it after one dose. Others take it for months before anything shows up.
The liver processes almost everything you swallow. When a drug or supplement messes with its normal function, liver cells get damaged. That’s when enzymes like ALT and AST leak into your blood. High levels mean something’s wrong. But here’s the catch: you might feel fine. No pain. No nausea. Just a vague sense of tiredness. That’s why it’s so dangerous.
There are three main patterns doctors look for:
- Hepatocellular injury: ALT levels jump above 5 times the normal range. This is the most common type. It happens fast-sometimes within days of starting a new antibiotic like amoxicillin-clavulanate.
- Cholestatic injury: Alkaline phosphatase and GGT rise sharply. This means bile isn’t flowing right. You might itch badly-really badly-before you turn yellow.
- Mixed pattern: Both types happen together. This often means the damage is more serious.
Take isoniazid, a TB drug. About 10% of people on it develop ALT levels over three times normal within three months. Most don’t notice anything until their blood test comes back. That’s why doctors monitor liver enzymes weekly for people on high-risk meds.
The Silent Symptoms You Might Be Ignoring
The biggest mistake people make? Assuming that if they feel okay, their liver is okay. But DILI doesn’t announce itself with a siren. It creeps in.
Here’s what to watch for-even if you think it’s "just stress":
- Dark urine: Like tea or cola. This isn’t dehydration. It’s bilirubin building up because your liver can’t process it.
- Yellow eyes or skin: Jaundice. It’s the classic sign-but by the time it shows up, damage is already advanced.
- Itching without a rash: Especially on the palms or soles. This is bile acids building up in your skin. It’s often the first warning.
- Pain under your right ribs: Not sharp, but a dull, constant ache. Like something’s swollen inside.
- Nausea or vomiting: Especially if it comes with fatigue and loss of appetite. Not flu. Not food poisoning.
- Unexplained fatigue: Not just tired. Exhausted. Like you’ve run a marathon for a week.
One patient from Bristol told me (in a support group) she had itching for two weeks on amoxicillin-clavulanate. Her GP said it was "just an allergic reaction." By the time she turned yellow, her ALT was 1,500 IU/L-15 times normal. She spent 12 days in hospital.
Which Medications Are Most Likely to Hurt Your Liver?
Not all drugs are equal. Some are well-known offenders. Others are sneaky.
Based on data from the UK’s Drug-Induced Liver Injury Network and the British Liver Trust, here are the top culprits:
| Drug Class | Examples | Typical Onset | Key Risk Factor |
|---|---|---|---|
| Antibiotics | Amoxicillin-clavulanate, flucloxacillin | 1-8 weeks | Flucloxacillin linked to HLA-B*57:01 gene-80x higher risk |
| Anticonvulsants | Valproate, carbamazepine | 2-12 weeks | Higher risk in children and those with metabolic disorders |
| NSAIDs | ibuprofen, diclofenac | Days to months | Long-term use increases risk |
| Acetaminophen | Paracetamol | 24-72 hours (overdose) | More than 3,000 mg/day can cause damage-even at therapeutic doses if combined with alcohol |
| Herbal Supplements | Green tea extract, kava, turmeric, aloe vera | 1 day to 12 months | 20% of UK DILI cases come from supplements. Green tea extract alone causes 37% of those |
Green tea extract is a shocker. People think it’s healthy. But concentrated extracts can be toxic. One 2023 case series in the Journal of Hepatology found 14 people in the UK with acute liver failure from weight-loss teas containing green tea extract. All were under 40. All were otherwise healthy.

When to Act-Right Now
You don’t need to wait for jaundice. If you’ve started a new medication-prescription or supplement-and you have any two of these symptoms within 8 weeks:
- Dark urine
- Right upper abdominal pain
- Nausea or vomiting
-then go to A&E. Don’t wait. Don’t call your GP tomorrow. Go today.
And if you’ve taken too much acetaminophen? If it’s been less than 8 hours, get to hospital immediately. N-acetylcysteine works best if given within that window. After 12 hours, the chance of saving your liver drops by half.
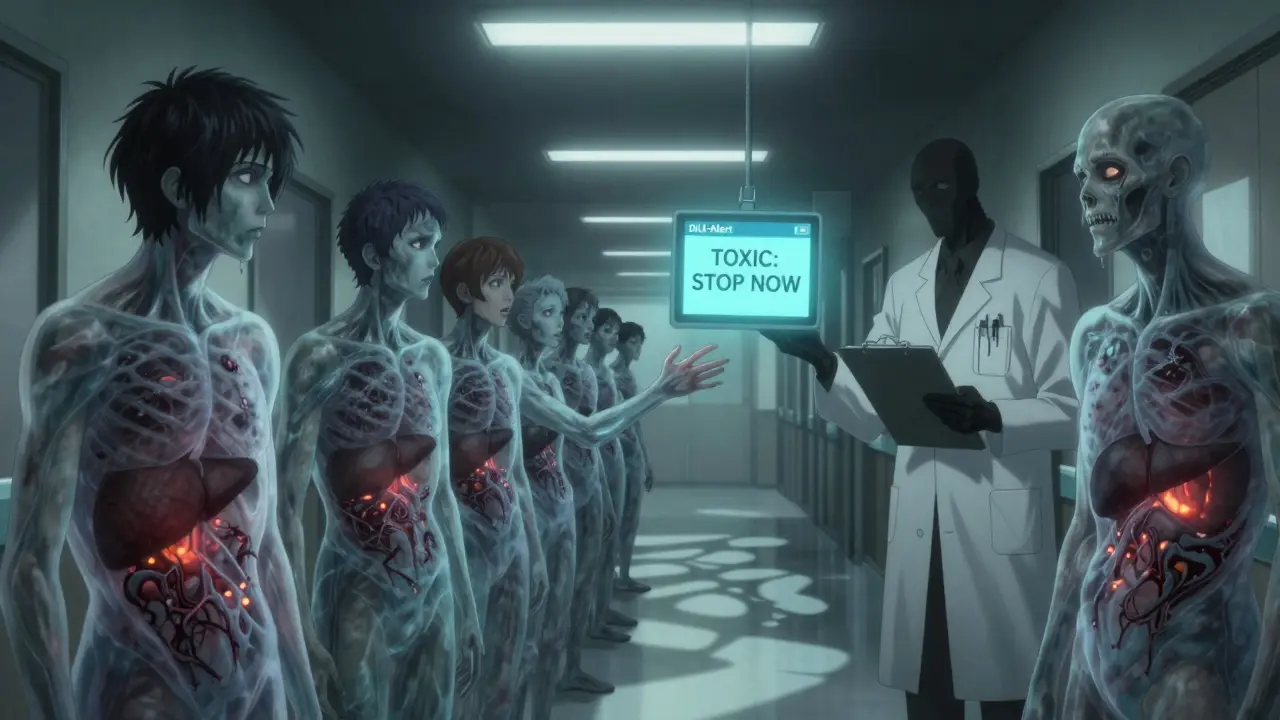
There’s also a tool called DILI-Alert-a smartphone app approved by the FDA in 2023-that lets you scan your medication labels and instantly see if they’re linked to liver injury. It’s free. It’s available in the UK. Use it.
Prevention Is Simple-If You Do It
Most cases of severe liver damage from meds are preventable. Here’s how:
- Know your doses: Never exceed 3,000 mg of acetaminophen a day. If you have liver disease, cut that to 2,000 mg. Read labels on cold medicines-they often contain hidden acetaminophen.
- Avoid alcohol with meds: Alcohol triples your risk of liver damage from painkillers, antibiotics, and even statins. Even one drink while on amoxicillin-clavulanate can be dangerous.
- Track everything: Write down every pill, capsule, tea, and powder you take. Include doses and start dates. Bring this list to every doctor visit.
- Question supplements: If your naturopath says "it’s detoxing" when you’re itching or yellow-you need a real doctor. Supplements aren’t regulated like drugs. No one checks their safety before they hit shelves.
- Ask about liver tests: If you’re on a long-term high-risk drug like isoniazid or valproate, ask for a liver enzyme test before you start-and every 4-6 weeks after.
Why So Many People Miss the Signs
Doctors aren’t always trained to spot DILI. A 2023 survey found only 42% of UK GPs could correctly name the top three drugs that cause liver damage. Patients don’t connect symptoms to meds because they trust prescriptions. They think "if my doctor prescribed it, it’s safe."
But here’s the truth: your liver doesn’t care if it’s a prescription or a supplement. It only cares if the chemical is toxic to it.
One Reddit user from Manchester wrote: "I took turmeric capsules for arthritis. My skin turned yellow. I went to my herbalist. She said it was "cleansing." Two weeks later, I was in ICU. My liver enzymes were 18x normal."
That’s the problem. We treat supplements like food. They’re not. They’re concentrated chemicals. And your liver has to process them all.
What Happens After Diagnosis?
Once DILI is suspected, the first step is always stopping the offending drug. That’s it. No fancy treatment. Just removal.
Most people recover fully if caught early. About 80% do. But if damage is advanced-like if you’ve developed liver failure-you may need a transplant. That’s not rare. DILI causes 13% of acute liver failures in the US, more than hepatitis A or B.
There’s no magic pill to fix it. No herbal cure. No detox tea. Just rest, time, and no more toxins.
Some people develop chronic liver issues. Others get scarring. A few need transplants. But none of that has to happen if you catch it in time.
What’s Changing Now?
There’s new hope. In 2023, researchers found that a tiny molecule called microRNA-122 rises in the blood within hours of liver damage-even before ALT spikes. It’s 92% accurate. Soon, hospitals might have a simple blood test that flags DILI before you even feel sick.
AI tools are also helping. One pilot system in London cut diagnosis time by 35% by cross-checking patient records with drug databases. That means fewer people wait weeks for answers.
But the biggest change? Awareness. The UK’s Medicines and Healthcare products Regulatory Agency (MHRA) now requires clearer warning labels on all herbal products. The FDA in the US has added black box warnings to antibiotics. That’s progress.
Still, the biggest threat isn’t drugs. It’s misinformation. People think "natural" means safe. It doesn’t. And too many are still taking high-dose supplements without knowing the risks.
Can over-the-counter painkillers cause liver damage?
Yes. Acetaminophen (paracetamol) is the most common cause of drug-related liver failure in the UK and US. Taking more than 3,000 mg a day-even spread out over several doses-can damage your liver. Many cold and flu remedies also contain acetaminophen, so you might be doubling up without knowing. Never take more than one product containing it at the same time.
Are herbal supplements safer than prescription drugs?
No. Herbal supplements are not safer. In fact, they cause 20% of all medication-related liver injuries in the UK. Products like green tea extract, kava, and turmeric are linked to severe liver damage. Unlike prescription drugs, supplements aren’t tested for safety before sale. What’s on the label isn’t always what’s inside. A 2022 study found 30% of herbal products contained unlisted chemicals that can harm the liver.
I feel fine. Do I still need liver tests if I’m on a high-risk medication?
Yes. Liver damage often has no symptoms until it’s advanced. If you’re taking drugs like isoniazid, valproate, or flucloxacillin, your doctor should order liver enzyme tests every 4-6 weeks. Waiting for symptoms means waiting too long. Early detection saves lives.
Can statins hurt my liver?
Statins can raise liver enzymes in about 1-2% of users, but serious injury is extremely rare-less than 1 in 10,000. The European Association for the Study of the Liver says these mild enzyme rises usually don’t need stopping the drug. However, if you develop jaundice, itching, or dark urine while on statins, get tested immediately. Don’t assume it’s "just a side effect."
How long does it take for the liver to recover after stopping the damaging drug?
Most people see improvement within weeks. ALT levels often drop by 50% in the first 2-4 weeks after stopping the drug. Full recovery can take 3-6 months. But if enzymes don’t start falling after 4 weeks, or if you have signs of liver failure (confusion, swelling, bleeding), you need urgent care. Some damage can be permanent.
Should I avoid all supplements to protect my liver?
Not all-but be cautious. Avoid high-dose extracts (like green tea extract capsules or concentrated turmeric pills). Stick to whole foods when possible. If you take supplements, choose ones with third-party testing (USP, NSF, or ConsumerLab labels). And always tell your doctor what you’re taking-even if you think it’s "just a vitamin."
What to Do Next
Here’s your action plan:
- Check every medication and supplement you’re taking. Write them down.
- Look up each one using the DILI-Alert app or the British Liver Trust’s online database.
- If you’re on a high-risk drug, ask your doctor for a liver enzyme test.
- Stop taking any supplement that causes itching, nausea, or fatigue.
- Never mix alcohol with painkillers or antibiotics.
- Keep a log. Date each new medication. Note how you feel.
Your liver doesn’t ask for permission. It doesn’t warn you. But if you know the signs, you can act before it’s too late.

Wow, this is eye-opening. I never thought my daily turmeric capsule could be quietly wrecking my liver. I’ll be checking my supplements tonight.
My dad had a near-miss with DILI from amoxicillin-clavulanate. He had itching for weeks and the doctor just said it was allergies. By the time they ran labs, his ALT was through the roof. He’s fine now but we’re all paranoid about meds now. Thanks for sharing this.
People think herbal = safe. No. It’s just unregulated poison with a yoga pose on the label. Green tea extract? More like liver wreck extract. Stop it.
As someone who reads peer-reviewed hepatology journals monthly, I’m frankly disappointed by the lack of nuance here. The DILI-Alert app is not FDA-approved-it’s merely FDA-registered. And microRNA-122 is still in validation trials, not clinical use. This reads like a BuzzFeed list dressed in medical jargon.
So let me get this straight-my ibuprofen is quietly murdering my liver, but my kombucha is fine? Right. I’ll just stop taking medicine and start drinking moonshine instead. Classic.
Thank you for this comprehensive and meticulously researched article. The distinction between hepatocellular and cholestatic injury is particularly well-articulated. I have forwarded this to my colleagues in the Department of Pharmacology at the Indian Institute of Medical Sciences, as it aligns closely with our ongoing work on drug metabolism variability in South Asian populations.
Let’s be real. Big Pharma knows this is happening. They bury the data. The FDA? A revolving door of ex-pharma execs. They don’t want you to know that your ‘safe’ meds are silent killers. That’s why they push ‘DILI-Alert’-it’s a distraction. The real fix? Ban all synthetic drugs. Go back to plants. Or better yet-stop trusting corporations with your liver. They’re not your friends.
I read this entire thing. Honestly, it’s a little too much. I mean, I take Tylenol for headaches, and now I’m supposed to panic every time I feel a little tired? This is fear-mongering wrapped in a white coat. People have been taking acetaminophen since the 1950s. If it was that dangerous, we’d all be dead by now. Also, why are you blaming supplements? People just want to feel better. Not everyone has time to track every capsule like a lab technician. Chill out.
I’m so grateful for this post. It’s so important to raise awareness about this. I’ve been on valproate for 12 years, and my doctor never mentioned liver tests. I just assumed I was fine because I didn’t feel sick. I’m scheduling a liver panel tomorrow. Thank you for the clear action plan. I’ve printed it out and taped it to my medicine cabinet. Every. Single. Day.
While the intent of this piece is commendable, the tone and structure are fundamentally flawed. The use of hyperbolic language such as "quietly becoming one of the leading causes" lacks statistical anchoring, and the anecdotal case from Bristol, while emotionally compelling, does not constitute evidence-based medicine. Furthermore, the reference to a "smartphone app approved by the FDA" is misleading; FDA registration is not equivalent to approval. I would urge the author to revise this with greater precision before disseminating to a lay audience.
Thank you for writing this. I’m a GP in Scotland, and I’ve seen too many patients come in too late. I’m sharing this with my whole practice. One thing I’d add: if you’re on any long-term medication, ask for a baseline liver test before you start-even if you feel fine. It’s not a big deal, it takes five minutes, and it could save your life. Also, if you’re taking supplements, write them down. I don’t care if it’s "just ashwagandha." Write it down. I’ve had patients tell me "I don’t take anything" and then pull out seven bottles from their purse. You’re not being dramatic-you’re being smart.