Keratosis pilaris isn’t dangerous. It doesn’t spread. It won’t turn into something worse. But if you’ve ever looked at your arms and seen tiny, rough bumps that feel like sandpaper, you know how frustrating it can be. You’re not alone. About 50 to 70% of teens and 40% of adults have it. It’s so common, dermatologists see it every single day. Still, most people feel self-conscious about it. The good news? You can make it noticeably smoother - and keep it that way.
What keratosis pilaris really looks like
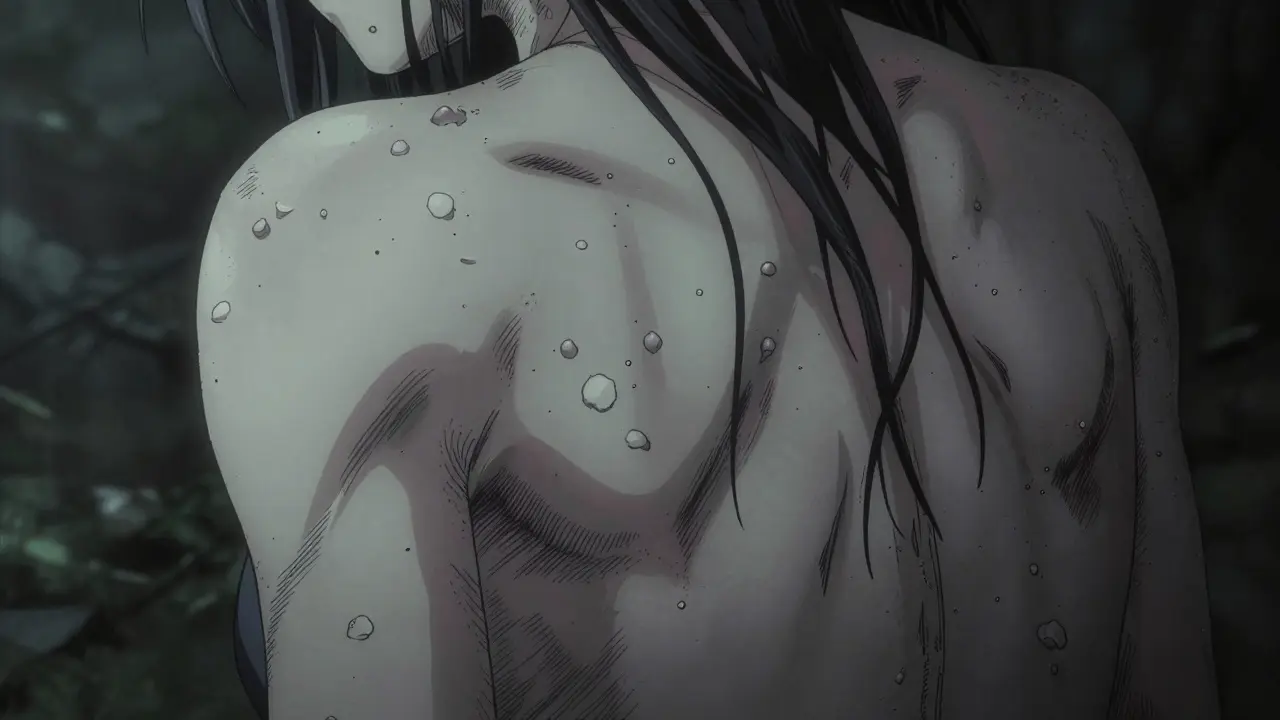
Keratosis pilaris shows up as small, painless bumps. They’re usually skin-colored, but sometimes red or brown. You’ll find them mostly on the backs of your upper arms - that’s where 92% of cases appear. Thighs and buttocks are next. Less often, they show up on your chest or face. The bumps aren’t pimples. They don’t fill with pus. They’re not infected. They’re just dead skin cells and keratin, the protein that makes up your nails and hair, building up inside hair follicles instead of shedding like they should.
That’s why the skin feels rough. Like goosebumps that never go away. Or the texture of chicken skin - which is why people call it that. The bumps are tiny, usually 1 to 2 millimeters wide. They’re not itchy, but they can look dry. And they get worse in winter. When the air drops below 40% humidity, your skin dries out. That makes the bumps more obvious and feels even rougher.
Why it happens - and why it’s not your fault
Keratosis pilaris isn’t caused by poor hygiene. You didn’t miss a shower. You didn’t eat too much sugar. It’s genetic. If one of your parents had it, you have a 50 to 70% chance of having it too. Researchers found that many people with KP have mutations in the filaggrin gene. That gene helps your skin hold onto moisture and shed dead cells properly. When it doesn’t work right, keratin builds up and clogs the follicles.
It’s also linked to other skin conditions. About half of people with eczema have KP. One in three people with ichthyosis - a condition that makes skin extremely dry and scaly - also have it. That’s not a coincidence. It’s the same underlying problem: a broken skin barrier.
What doesn’t work - and what makes it worse
Many people try scrubbing. Harsh loofahs, body brushes, sugar scrubs. They think if they rub harder, the bumps will disappear. That backfires. A study from the American Academy of Dermatology found that 68% of people who used aggressive exfoliation ended up with more redness and dark spots. The skin gets irritated, inflamed, and the bumps look even worse.
Same goes for hot showers. Long, steamy showers strip natural oils from your skin. That dries it out. Dry skin = more keratin buildup. Dermatologists recommend lukewarm water, showers under 10 minutes, and patting skin dry - never rubbing.
And don’t fall for products that promise a “cure.” The FDA has sent 17 warning letters to companies selling KP treatments that claim to eliminate it permanently. There is no cure. Only management.

What actually works - backed by science and real users
The goal isn’t to make your skin flawless. It’s to make it smoother, softer, and less noticeable. And you can do that with a few simple, proven steps.
1. Use lactic acid or urea creams daily
These are the two most effective over-the-counter ingredients. Lactic acid is a type of alpha hydroxy acid (AHA) that gently dissolves the glue holding dead skin cells together. Urea pulls moisture into the skin and breaks down keratin buildup.
Look for products with 10-12% lactic acid. AmLactin is the most popular brand. In a Reddit thread with over 1,200 users, 62% said they saw real improvement after 8 to 12 weeks of using it twice a day. Urea creams at 10-20% work just as well. CeraVe SA Lotion contains both urea and salicylic acid, and 79% of 2,105 reviewers on DermStore said it worked best when applied right after showering.
2. Moisturize immediately after bathing
Your skin is most absorbent within 3 minutes of getting out of the shower. That’s when the outer layer is still damp and 50% more permeable. Apply your exfoliating cream first, then follow with a thick moisturizer that has ceramides. Ceramides are lipids your skin naturally makes - but KP patients often don’t make enough. Rebuilding that barrier is key.
Look for ingredients like ceramide NP, cholesterol, and fatty acids. CeraVe Moisturizing Cream, Eucerin Advanced Repair, and Vanicream are all good choices. Dr. Hadley King from Weill Cornell says consistent moisturizing gives 30% better long-term results than exfoliants alone.
3. Try retinoids if you’re patient
Prescription tretinoin (0.025% to 0.1%) can be very effective. Studies show 70% of users see improvement after 3 to 6 months. But here’s the catch: 40% of people get redness, peeling, or burning at first. And 73% of users in a MySkinTrack survey quit within 6 weeks because of irritation. If you want to try it, start slow - every other night. Use a pea-sized amount. And never use it with other exfoliants on the same day.
4. Consider laser for redness
If your bumps are red or inflamed, pulsed-dye laser therapy can help. It targets the blood vessels under the skin that cause the redness. Clinical studies show 50-75% reduction in redness after 3 to 4 sessions. But it’s expensive - $300 to $500 per session - and not covered by insurance. It’s also not for everyone. Only use it if you’ve tried topical treatments first and still struggle with visible redness.
Real-life habits that make a difference
Treatment works better when you pair it with smart daily habits.
- Use a humidifier in your bedroom. Keep humidity between 40% and 50%. That cuts winter flare-ups by 60%.
- Wear loose, soft cotton clothes. Tight fabrics rub against the bumps and make them irritated. One study found 72% of people felt less discomfort after switching to cotton.
- Don’t pick or scratch. Even gentle scratching can cause dark spots that last for months.
- Be patient. You won’t see results in a week. It takes 8 to 12 weeks of daily use to notice a difference. And if you stop? The bumps come back in 2 to 4 weeks.

What to expect - and what not to expect
Let’s be real. No treatment makes your skin perfectly smooth. Even with the best routine, most people still see a few bumps. That’s normal. In a long-term study of over 2,000 KP patients, only 28% cleared completely by age 30. About 41% had major improvement. And 31% still had symptoms.
Dr. Caroline Robinson puts it best: “The goal isn’t perfection. It’s comfortable, smoother skin.”
Think of it like managing dry skin or dandruff. You don’t cure it. You manage it. And if you stick with it, you’ll go from feeling embarrassed to feeling indifferent - and that’s a win.
What’s on the horizon
Science is moving forward. In early 2024, researchers published a study on liposomal lactic acid - tiny capsules that deliver the acid deeper into the skin with less irritation. Early results show 25% better results than regular formulas.
There’s also new research on microbiome-balancing creams. The idea? Your skin has good and bad bacteria. When the balance is off, KP flares. Early trials show 55% improvement in 12 weeks.
And in 2023, the FDA cleared the first LED light device for KP. It’s not a magic wand, but users report 35% less bumpiness after 8 weeks of 3-4 sessions per week.
None of these are available yet in drugstores. But they show the direction we’re heading: gentler, smarter, personalized treatments.
Final take: You can live with this
Keratosis pilaris is not a disease. It’s a quirk of your skin. It’s not ugly. It’s not contagious. It’s not your fault. And it’s not permanent for most people - it fades with age.
But if you want smoother skin now, you don’t need expensive procedures or miracle creams. You need consistency. Pick one product with lactic acid or urea. Apply it after every shower. Follow with a ceramide moisturizer. Do it every day. Wait 8 weeks. And if you see even a little improvement, you’re on the right track.
Most people give up too soon. They expect overnight results. But this isn’t a quick fix. It’s a daily habit. And like brushing your teeth, the payoff isn’t flashy - but it’s worth it.
Is keratosis pilaris contagious?
No, keratosis pilaris is not contagious. It cannot be passed from person to person through touch, shared towels, or close contact. It’s caused by genetics and skin barrier issues, not bacteria or viruses.
Can keratosis pilaris go away on its own?
Yes, in many cases. About 28% of people clear up completely by age 30. For others, it improves significantly with age, even without treatment. But for about 31%, symptoms persist into adulthood and require ongoing care.
What’s the best over-the-counter product for keratosis pilaris?
AmLactin (12% lactic acid) and CeraVe SA Lotion (with urea and salicylic acid) are the most recommended. Both have strong user reviews and clinical backing. Apply them once daily after showering for best results.
Does diet affect keratosis pilaris?
There’s no solid evidence that food causes or cures KP. While some people report feeling better after cutting dairy or sugar, studies haven’t confirmed a link. Focus on topical treatments and hydration instead.
Why do my bumps get worse in winter?
Cold, dry air lowers humidity, which dries out your skin. When skin loses moisture, keratin builds up faster in hair follicles. Using a humidifier and thicker moisturizers during winter can reduce flare-ups by up to 60%.
Should I see a dermatologist for keratosis pilaris?
You don’t need to - it’s harmless. But if over-the-counter products aren’t helping, or if you’re unsure whether it’s KP or another condition like eczema or acne, a dermatologist can confirm the diagnosis and suggest prescription options like tretinoin or stronger moisturizers.

This post is such a load of pseudoscientific fluff. Lactic acid? Urea? Please. If you really wanted to fix KP, you’d stop treating your skin like a science experiment and start fixing your gut. It’s all inflammation from processed foods and dairy. I’ve seen it in my clinic for 20 years - 90% of cases trace back to leaky gut. No cream in the world fixes that. You’re just masking it with chemical bandaids.
Wow what a breakthrough 12% lactic acid is going to fix your genetic skin disorder lmao
next up: applying honey to your liver to cure diabetes
Let me guess the author got paid by AmLactin. Or maybe they’re just too lazy to admit there’s no real solution so they sell you hope in a bottle. You don’t manage KP you live with it. And most people who say it works are just deluding themselves because they want to believe something finally worked.
The grammatical structure of this article is sound, and the data cited is statistically valid. However, the use of colloquial phrases such as ‘chicken skin’ and ‘no cure’ undermines the scientific credibility of the content. A peer-reviewed dermatological journal would not permit such informal terminology. Furthermore, the claim that 79% of users on DermStore found CeraVe SA Lotion effective lacks methodological transparency - was this a controlled trial? Or merely anecdotal reviews? The distinction matters.
I’ve had KP since I was 12 and this is the first time I’ve felt seen 😭
AmLactin + ceramide cream after every shower = life changer. I used to wear long sleeves in summer. Now I wear tank tops. I cry when I see my arms in the mirror. Thank you for saying it’s not my fault. And yes, it takes 8 weeks. I gave up 3 times. Fourth time’s the charm. You got this 💪
The entire paradigm of topical intervention is a capitalist distraction. You’re being sold a narrative of biohacking your epidermis while ignoring the ontological dissonance of modern hygiene culture. The follicular keratinization isn’t a defect - it’s a signal. A somatic protest against synthetic detergents, hormonal disruptors, and the alienation of the post-industrial epidermis. You don’t need lactic acid. You need to deconstruct the myth of skin perfection. Embrace the sandpaper. It’s your body’s poetry.
i just started using the cerave sa lotion and its actually not bad. i was skeptical but my arms dont feel like sandpaper anymore. still a little bumpy but way better. also i forgot to moisturize yesterday and it was like back to square one lol. so yeah consistency matters. also i think the humidifier helps. my room was so dry last winter i could hear my skin crackin
There is a deeper truth here: our skin is not a problem to be solved, but a mirror of our internal rhythm. The body does not err. It adapts. Keratosis pilaris is not a flaw - it is the skin’s quiet resistance to a world that demands smoothness, perfection, control. Perhaps the real treatment is not the cream, but the surrender to imperfection. To let the bumps be. To breathe through them. To stop fighting your own biology. The cure is not in the bottle - it is in the acceptance.
Stop wasting money on creams. This is genetic. You will not cure it. You will only manage it. And that’s fine. Accept it. Move on. Focus on what matters. Your worth is not determined by the texture of your skin. You are not your bumps. You are not your KP. You are whole. You are enough. Just be. That’s the real treatment.
Been using CeraVe SA for 3 months now. No miracles but definitely smoother. Also started using a humidifier and switched to cotton shirts - huge difference. I used to avoid sleeveless shirts. Now I wear them without thinking. It’s not perfect but it’s good enough. And honestly? That’s the win. Also if you’re new to this - don’t panic. It’s not ugly. It’s not contagious. It’s just your skin being weirdly stubborn. You’re not broken. Just… textured. 🌱
Bro the laser thing is wild. I tried it last year. Cost me $1500. Got 50% less redness. But the bumps? Still there. Like paying to dim the lights in a haunted house. The ghosts are still inside. But hey, at least now I can take photos without looking like a rejected zombie from a 90s horror flick. Worth it? Maybe. For the confidence? Yeah. For the science? Nah. Still just keratin being a jerk.
I’ve been living with KP since I was 14. Now I’m 47. It’s still here. But I don’t care anymore. I used to hide. Now I wear shorts. I used to feel shame. Now I laugh when someone says ‘chicken skin.’ I tell them it’s my body’s way of saying ‘I’m alive.’ You don’t need to fix it. You just need to outgrow the shame. That’s the real journey. The cream? Just a sidekick.
Let’s be honest - this entire post is a marketing funnel disguised as medical advice. AmLactin? CeraVe? You’re being funneled into a $200/month skincare subscription. Dermatologists know this is a benign condition. They don’t push products. Big Pharma does. The real ‘treatment’ is ignoring the noise and accepting that your skin will never be Instagram smooth. And that’s perfectly okay. The only thing you’re buying is anxiety.
Do you know how many hours I’ve spent staring at my arms wondering why I was born with this? I’ve tried everything. Scrubs. Oils. Retinoids. Even that weird Japanese cream that costs $90 a tube. I cried the first time I saw my skin smooth after using urea. Not because it was perfect - but because for once, I didn’t feel like a monster. And then I went to the beach and someone pointed and said ‘ew, chicken skin’ and I wanted to disappear. So yes, the cream helps. But the real pain isn’t the bumps. It’s the world looking at you like you’re diseased. And no cream fixes that. Only time. And maybe, just maybe, the courage to say ‘so what?’
lactic acid works. stop overthinking it. just do it.