
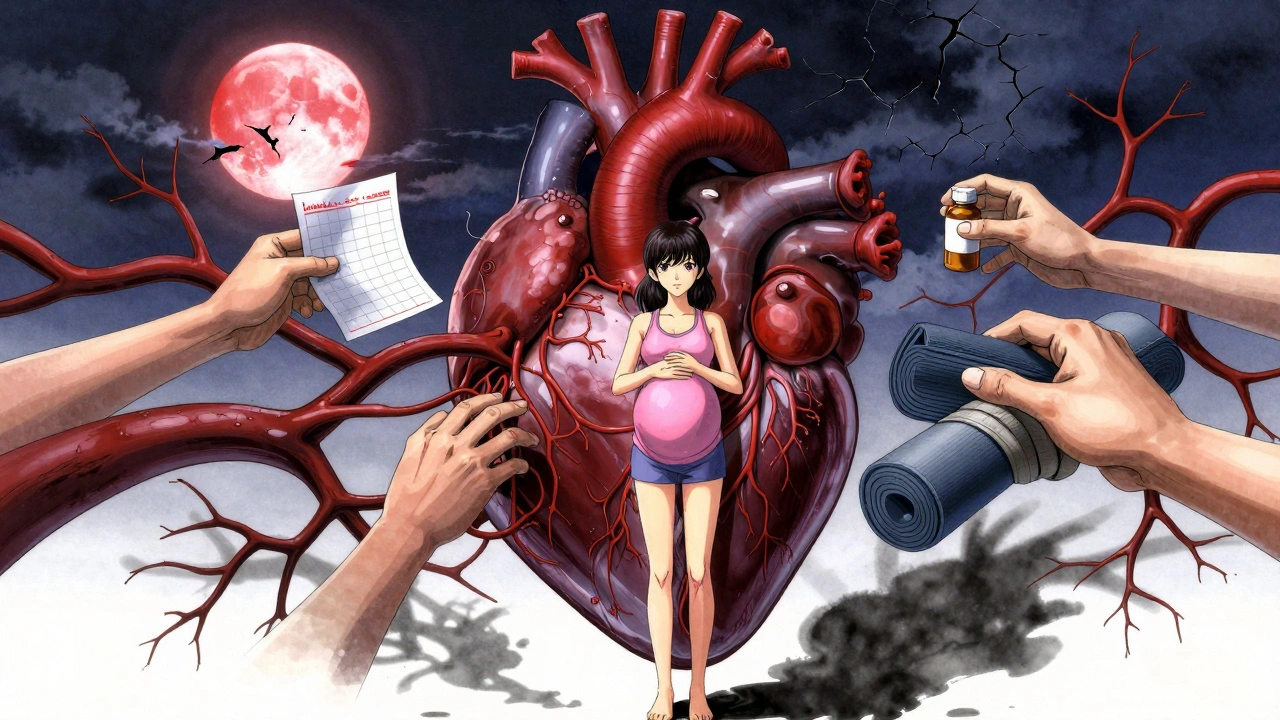
Heart disease kills women more than all cancers combined. Yet most women don’t realize it’s their biggest health threat. In the U.S., about 1 in 5 female deaths is caused by heart disease - that’s over 307,000 women every year. But here’s the problem: many don’t recognize the signs until it’s too late. Why? Because women’s heart attacks don’t always look like the ones you see in movies.
What Heart Attack Symptoms Look Like in Women
The classic image of a heart attack - clutching your chest, screaming in pain - is mostly a male experience. For women, symptoms are often quieter, stranger, and easier to dismiss. You might feel like you’ve been hit by a truck, but no one can see the injury.
Forty-two percent of women having a heart attack report sudden, unexplained shortness of breath - even when they’re sitting still. Thirty-six percent feel nauseous or vomit. Nearly a third experience extreme fatigue, so bad they can’t make their bed or walk to the mailbox. One in four feel dizziness or lightheadedness. And 45% feel pain in their arms, jaw, neck, or back - not their chest.
Even when women do feel chest discomfort, it’s rarely the crushing, knife-like pain men describe. Instead, they report pressure, tightness, or a burning sensation. Some say it feels like indigestion. Others say it’s like a heavy weight sitting on their chest. And sometimes, there’s no chest pain at all. In fact, 43% of women who have heart attacks don’t have any chest pain. That’s why so many go to the ER thinking they have the flu, anxiety, or acid reflux - and get sent home.
One of the most overlooked symptoms is what doctors call “vital fatigue.” It’s not just being tired. It’s waking up exhausted after a full night’s sleep. It’s needing to sit down after brushing your hair. It’s canceling plans because you simply can’t move. In one Yale study, 71% of women who had heart attacks reported this level of fatigue in the weeks before their event - but only 12% connected it to their heart.
Why Women’s Hearts Are Different
Women aren’t just smaller men when it comes to heart health. Their bodies work differently. Their arteries are narrower. Their heart muscle responds differently to stress. Hormones play a role - especially after menopause, when estrogen drops. But even younger women face unique risks.
Conditions like spontaneous coronary artery dissection (SCAD) - where a tear forms in a heart artery - happen mostly in women under 50, often without traditional risk factors like high cholesterol or smoking. Stress-induced cardiomyopathy, also called Takotsubo syndrome, mimics a heart attack but is triggered by extreme emotional stress - like the death of a loved one or a divorce. It’s far more common in women.
Microvascular disease affects the tiny arteries that branch off the main heart vessels. It’s more common in women and doesn’t show up on standard tests like angiograms. Instead, it causes ongoing fatigue, shortness of breath, and chest discomfort during daily activities - symptoms that doctors often mistake for anxiety or aging.
And then there’s silent heart attacks. Women over 65 are 34% more likely than men to have one without knowing it. No pain. No warning. Just unexplained fatigue, nausea, or a strange feeling that something’s off. These silent events damage the heart slowly - and increase the risk of future, more deadly events.
Why Diagnosis Is So Often Wrong
When women show up at the ER with symptoms like fatigue, nausea, or jaw pain, they’re more likely to be told they’re anxious, stressed, or having a panic attack. A 2022 study in JAMA Internal Medicine found that 68% of women with cardiac symptoms were initially misdiagnosed as having psychological issues.
Under-55 women are seven times more likely than men to be sent home from the ER without proper testing. And the cost? A 50% higher chance of dying within a year after a misdiagnosed heart attack. That’s not just a gap in awareness - it’s a gap in care.
Doctors aren’t always trained to look for women’s symptoms. Medical textbooks still focus on the male model. Clinical trials have historically included mostly men - women made up only 38% of participants in major heart studies, even though they’re half the population. As a result, diagnostic tools like stress tests and EKGs were designed for male physiology. They miss up to 30% of heart problems in women.
Even when tests are done, women’s results are often misinterpreted. A normal EKG doesn’t mean a healthy heart - especially if you have microvascular disease. Blood tests for heart enzymes can be normal in women even during a heart attack. That’s why doctors need to look at the whole picture: symptoms, history, and risk factors - not just one test.

Key Risk Factors Women Can’t Ignore
High blood pressure, high cholesterol, and smoking are risks for everyone. But women have unique risk factors that many don’t know about.
- Pregnancy complications: Preeclampsia - high blood pressure during pregnancy - increases future heart disease risk by 80%. Gestational diabetes and preterm delivery also raise your risk.
- Menopause: After menopause, estrogen drops. That means LDL (bad) cholesterol rises, HDL (good) cholesterol falls, and blood pressure tends to climb. The risk of heart disease jumps sharply after 55.
- Autoimmune diseases: Lupus, rheumatoid arthritis, and other autoimmune conditions are more common in women and double the risk of heart disease.
- Chronic stress and depression: Mental stress triggers angina in women 37% more often than in men. Depression is linked to a 50% higher risk of heart attack in women.
- Polycystic ovary syndrome (PCOS): Women with PCOS have higher insulin resistance, higher blood pressure, and more abdominal fat - all major heart disease risks.
Family history matters, too. If your mother or sister had heart disease before age 65, your risk doubles. But even without family history, these female-specific risks can put you in danger.
What You Can Do: Prevention and Early Action
Heart disease isn’t inevitable - even with risk factors. The key is knowing your numbers and acting early.
Start with a simple checklist:
- Know your blood pressure. Aim for under 120/80. Anything over 130/80 needs attention.
- Check your cholesterol. LDL should be under 100. If you have other risks, aim for under 70.
- Test for diabetes. Fasting blood sugar over 100 means you’re at risk.
- Track your menstrual and pregnancy history. Did you have preeclampsia? Gestational diabetes? Early menopause? Tell your doctor.
- Don’t ignore fatigue. If you’ve been unusually tired for more than two weeks - especially with shortness of breath - get checked. It could be the first sign.
Exercise isn’t just about weight. Walking 30 minutes a day, five days a week, cuts heart disease risk by 30%. Strength training twice a week helps control blood pressure and insulin levels. Even small changes matter.
Stop smoking. Quitting before age 40 reduces your heart disease risk to nearly the same level as someone who never smoked. And if you’re on birth control pills, talk to your doctor - smoking while on the pill increases your stroke and heart attack risk dramatically.
Manage stress. Yoga, meditation, deep breathing - these aren’t just nice to have. They’re medical tools. Chronic stress raises cortisol, which spikes blood pressure and inflammation. Women who practice daily stress-reduction techniques cut their heart attack risk by nearly 40%.
When to Demand Immediate Care
If you have three or more of these symptoms - even if they’re mild - don’t wait. Don’t call your doctor tomorrow. Go to the ER now:
- Unexplained fatigue (especially if it’s new and severe)
- Shortness of breath during normal activities
- Nausea or vomiting without a stomach bug
- Pain in your jaw, neck, shoulder, or back
- Lightheadedness or sudden dizziness
Don’t let anyone tell you it’s just anxiety. Don’t let them send you home because your EKG looks normal. Ask for a cardiac troponin test. Ask for a stress echo or coronary CT angiogram if your symptoms persist. If your doctor says no, ask for a referral to a women’s heart clinic.
Hospitals with certified Women’s Cardiovascular Centers of Excellence have 25% fewer diagnostic delays for women. They know the signs. They use gender-specific protocols. They don’t dismiss fatigue as stress.
The Future Is Changing - But You Can’t Wait
Progress is happening. The FDA approved the Corus CAD test in 2020 - a blood test that analyzes gene patterns to detect heart disease in women with 88% accuracy. The NIH launched the RENEW initiative in 2023, investing $150 million to study women’s heart health. AI tools are being trained to recognize female symptom patterns - and could cut misdiagnosis rates by 40% in the next five years.
But these advances won’t help you if you don’t speak up. You are your own best advocate. If you feel something’s wrong - even if you can’t explain it - trust your gut. Heart disease doesn’t always scream. Sometimes, it whispers. And if you’re not listening, you might miss it.
Women are not just surviving heart disease - they’re learning to fight it. But the first step isn’t medication. It’s awareness. The second is action. Don’t wait for a crisis. Start today. Know your body. Know your risks. And never, ever ignore the quiet signs.
Do women have different heart attack symptoms than men?
Yes. While chest pain is common in both, women are more likely to have symptoms like extreme fatigue, nausea, shortness of breath, jaw or back pain, and dizziness - often without chest discomfort. About 43% of women have heart attacks without any chest pain at all.
Is heart disease really the top killer of women?
Yes. Heart disease causes about 1 in every 5 female deaths in the U.S. - more than all cancers combined. Yet only 44% of women knew this was their biggest health threat as of 2019, according to the American Heart Association.
Can stress cause a heart attack in women?
Yes. Mental stress triggers angina and heart attacks in women 37% more often than in men. Extreme emotional events can even cause Takotsubo syndrome - a condition that mimics a heart attack but is caused by stress, not blocked arteries.
What should I do if I think I’m having a heart attack?
Call 911 immediately. Don’t drive yourself. Don’t wait to see if it goes away. Even if you’re unsure, get checked. Women are more likely to be sent home with a misdiagnosis - so insist on cardiac testing if symptoms persist.
Are standard heart tests accurate for women?
Not always. Traditional stress tests and EKGs were designed on male data and miss up to 30% of heart problems in women. Tests like the Corus CAD blood test or coronary CT angiogram are more accurate for detecting microvascular disease and other female-specific conditions.
Can pregnancy affect my heart health later in life?
Yes. Complications like preeclampsia, gestational diabetes, or preterm birth increase your long-term risk of heart disease by 50-80%. Your pregnancy history is a critical part of your heart health profile - tell your doctor.
What’s the best way to prevent heart disease as a woman?
Know your numbers: blood pressure, cholesterol, and blood sugar. Stay active - even 30 minutes of walking daily helps. Quit smoking. Manage stress with yoga, meditation, or therapy. Get checked if you feel unusual fatigue, shortness of breath, or unexplained nausea - especially if you’ve had pregnancy complications or are postmenopausal.

My mom had a heart attack and didn't have chest pain at all. Just felt like she'd been run over by a bus for three days. Doctors kept telling her it was anxiety. She almost died because no one listened. This post? Spot on.
The microvascular dysfunction data is underappreciated in clinical practice. Standard angiography misses up to 40% of cases in premenopausal women due to diffuse endothelial dysfunction. The coronary flow reserve metrics from PET scans are far more sensitive, yet rarely ordered unless there's a known autoimmune comorbidity. We need gender-specific diagnostic algorithms integrated into EMRs.
THIS. I had three years of unexplained fatigue, nausea, and jaw pain. My PCP said I was just "stressed from work." I went to the ER again after collapsing at the grocery store. Turned out I had SCAD. No smoking. No high cholesterol. Just a 37-year-old woman who got lucky. Please, if you're reading this and feel off - don't wait.
Also, if you're a doctor reading this - please stop dismissing women's symptoms as "anxiety." We're not drama queens. We're just trying to survive.
my aunt died from a silent heart attack. no warning. just didn't wake up. she was 58. no history of heart problems. just tired a lot. they said it was "aging."
Thank you for writing this. I’ve been too scared to say it out loud, but I’ve had this constant heaviness in my chest since my mom passed. My doctor said it was grief. But what if it’s not? I’m getting a stress echo next week. I don’t want to wait until it’s too late. 💙
India has same problem. Women ignore symptoms because they think heart disease is for men or old people. My sister had preeclampsia, then ignored fatigue for 2 years. Now she has microvascular disease. Doctors here don’t even know about SCAD. Need more awareness.
Wow, another "women are special snowflakes" article. Next they’ll say we need different stairs because our hips are wider. Can we just use the same damn EKGs and stop pretending biology is a political issue?
Y’all need to hear this. I’m 42, had gestational diabetes, now I’m postmenopausal. Started walking 30 mins a day. Lost 18 lbs. BP dropped from 145/92 to 118/76. I’m not a doctor, but I’m alive because I listened. You can too. Start today. Just walk. 🚶♀️💪
My mom’s cardiologist finally ordered a Corus CAD test after she kept saying "something’s wrong." Normal EKG, normal troponin. But the gene panel flagged high risk. Turned out she had microvascular disease. She’s alive because someone believed her. Don’t let anyone make you feel crazy for pushing for answers.
I used to think heart disease was for old men in suits. Then my sister had a heart attack at 39. No chest pain. Just couldn’t breathe while folding laundry. She’s on meds now. I quit smoking. I walk every day. I talk to my doctor about my pregnancy history. This isn’t fear-mongering - it’s survival. We owe it to our mothers, sisters, daughters.
Big Pharma and the AMA are hiding this. Why? Because if women knew their hearts are different, they’d demand better tests. And then insurance companies would have to pay for real diagnostics. Meanwhile, women are dying so Wall Street can keep profiting off statins and bypasses. Wake up. This is a system failure.
Here’s the truth: 70% of women who die from heart disease had no prior diagnosis. That’s not coincidence. That’s negligence. If you’re over 40, get a coronary calcium scan. If you’ve had preeclampsia, tell your doctor. If you’re tired all the time - don’t shrug it off. Your heart is talking. Are you listening?
They told me my symptoms were "hormonal." I had a 5-year history of fatigue, jaw pain, and sudden nausea. They called it perimenopause. Turns out I had a 90% blocked artery. The ER doctor said "you’re too young for this." I screamed at him. He called security. I had a heart attack 3 days later. This isn’t a medical issue - it’s a patriarchy issue.
While the clinical data presented is statistically valid, the rhetorical framing exhibits a concerning trend of pathologizing normal female physiology. The conflation of fatigue with cardiac pathology risks overmedicalization. The data does not support universal screening for microvascular disease in asymptomatic women - yet this narrative implies it. Caution is warranted.
Re: the Corus CAD test - it’s not perfect. Sensitivity is 88%, but specificity drops to 72% in women with chronic inflammation. That means false positives are common in autoimmune patients. We need to combine it with high-sensitivity CRP and NT-proBNP for better predictive value. The FDA approval was a start, but it’s not a silver bullet.