Generic Equivalence: What It Really Means When You Switch Medications
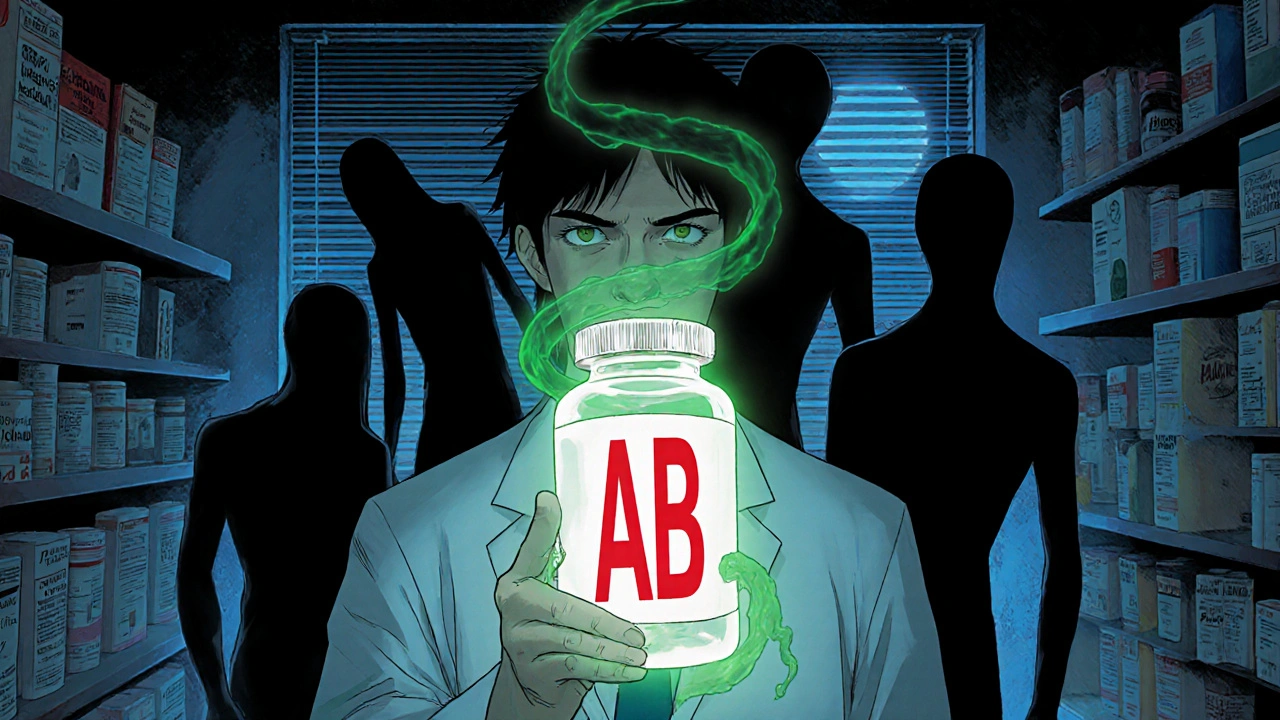
When you pick up a prescription and see a different name on the bottle, you might wonder: generic equivalence, the legal and scientific standard that says a generic drug must perform the same as the brand-name version in the body. Also known as pharmaceutical equivalence, it's the baseline requirement before a generic can even be sold in the U.S. But here’s the catch—having the same active ingredient doesn’t always mean the same result. The FDA says generics must match the brand in strength, dosage form, and route of administration. That’s pharmaceutical equivalence. But what you really care about is therapeutic equivalence, whether the drug produces the same clinical effect and safety profile in patients. And that’s where things get messy.
Some drugs are forgiving. If you switch from brand-name ibuprofen to a generic, you won’t notice a difference. But others? Not so much. warfarin, a blood thinner with a narrow therapeutic index, is one of them. Tiny changes in how the body absorbs the drug—even from one generic to another—can cause your INR to spike or drop. That’s why doctors monitor it closely after a switch. The same goes for anticonvulsants, like phenytoin, where even 10% variation in absorption can trigger seizures or toxicity. These aren’t theoretical risks. Real people have ended up in the ER because of a generic switch that wasn’t handled right.
And it’s not just about the pill itself. Where it’s made matters. Most generic drugs are produced overseas, and FDA oversight, while improving, still struggles to keep up with the volume of inspections needed. A drug might pass lab tests but still have inconsistent release patterns in the body. That’s why some pharmacists won’t substitute certain generics without the doctor’s okay. It’s not about brand loyalty—it’s about safety.
You don’t need to fear generics. They save billions and work perfectly for most people. But understanding generic equivalence means knowing when to ask questions. If you’re on a drug with a narrow window for error—like warfarin, lithium, or thyroid meds—don’t assume all generics are equal. Ask your pharmacist if the new bottle is the same batch as before. Check your blood levels if you’re on something critical. And if you feel different after a switch? Speak up. Your body notices before the lab does.
Below, you’ll find real-world guides on how generic switches affect people, what the FDA really checks, and which medications demand extra caution. No fluff. Just what you need to know to stay safe—and save money—without guessing.
How Pharmacists Verify Generic Equivalence: Practice Standards
Pharmacists use the FDA's Orange Book to verify that generic drugs are therapeutically equivalent to brand-name versions, ensuring safe and legal substitutions. This process relies on strict bioequivalence standards and state laws to protect patient safety.
read more