More than 95% of people told they’re allergic to penicillin aren’t actually allergic. Yet they’re still avoiding it-and so are their doctors. This isn’t a minor mistake. It’s a nationwide health problem that’s making antibiotics less effective, raising costs, and putting patients at risk. If you’ve been told you’re allergic to penicillin-or any antibiotic-based on a childhood rash, a family story, or a vague reaction from years ago, you might be carrying a false label. And that label could be costing you better treatment options, longer hospital stays, and even your life.
Why False Allergy Labels Are Dangerous
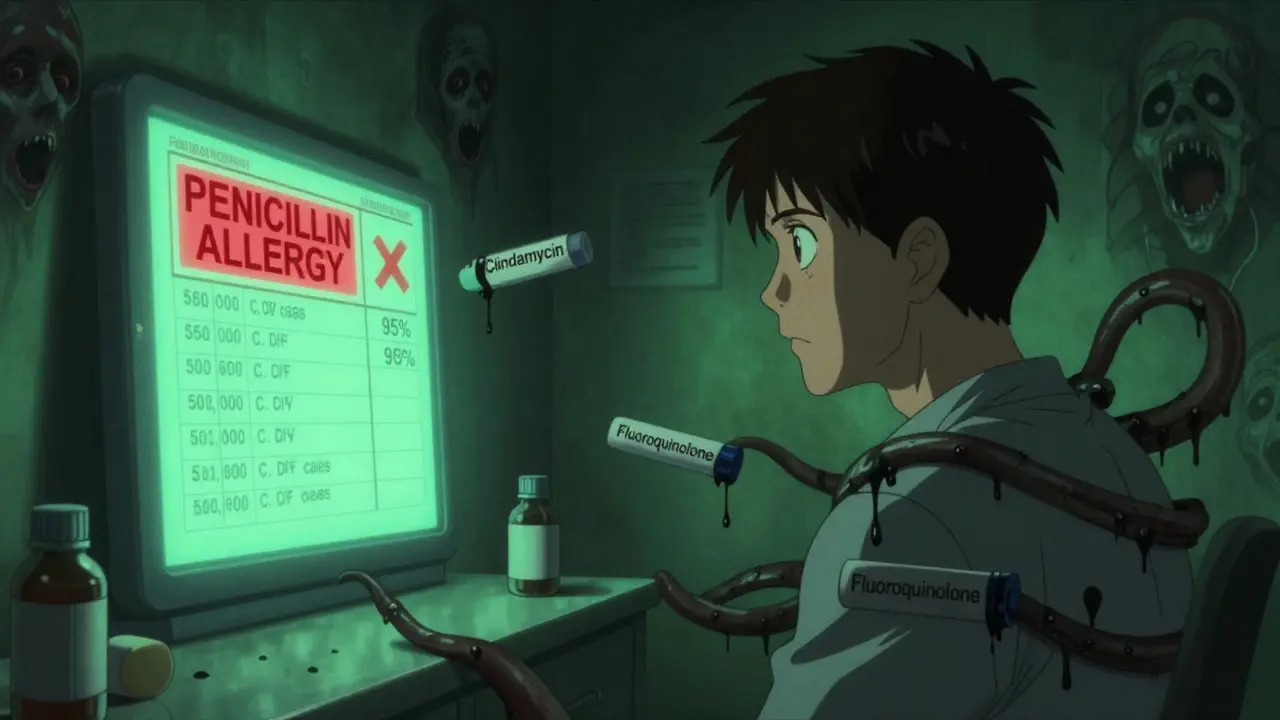
When someone is labeled allergic to penicillin, doctors can’t use it. Even if the label is wrong. That means they turn to other antibiotics-ones that are broader, stronger, and more expensive. These drugs don’t just cost more. They’re also more likely to cause side effects like severe diarrhea from C. diff infections, or to push bacteria toward dangerous resistance. In the U.S., about 10 to 15% of hospitalized patients have a penicillin allergy label. But studies show only 1 to 2% of those people have a true IgE-mediated allergy. That means roughly 9 out of every 10 people with that label are mislabeled. The result? Hospitals use fluoroquinolones 28% more often and clindamycin 69% more often in these patients. Both are linked to higher rates of MRSA and drug-resistant E. coli. The CDC estimates that false penicillin labels contribute to 50,000 extra C. diff cases every year in the U.S.-and $650 million in added healthcare costs. It’s not just about money. It’s about outcomes. People with false allergy labels are more likely to be readmitted to the hospital, stay longer, and get worse infections because they’re stuck with second-line drugs that don’t work as well.How Do You Know If Your Allergy Label Is Wrong?
Most people don’t know how they got the label. Maybe it was a rash at age 6. Maybe your mom said you were allergic. Maybe a nurse wrote it down after you felt nauseous during a dental procedure. None of those are proof of a true allergy. True drug allergies involve the immune system. They cause symptoms like hives, swelling, trouble breathing, or anaphylaxis-usually within minutes to an hour after taking the drug. A mild rash that shows up days later? That’s often not an allergy. Nausea? That’s a side effect. Diarrhea? That’s a common antibiotic reaction, not an allergy. The key question isn’t whether you had a reaction. It’s whether it was a real immune response. And the only way to know for sure is to get tested.How Drug Allergy Testing Works
There are three main ways to test for a true drug allergy-and they’re all safer than you think. 1. Skin TestingThis is the first step for most people. A tiny amount of the drug is placed under the skin using a prick or a small injection. If you’re truly allergic, a red, itchy bump appears within 15 to 20 minutes. Skin tests for penicillin are highly accurate-over 98% negative predictive value. That means if the test is negative, you’re almost certainly not allergic. 2. Drug Provocation Test (DPT)
If skin testing is negative-or if you’re low-risk and your doctor recommends skipping it-you’ll be given a small dose of the drug, then gradually increased under supervision. You’re watched for 30 to 60 minutes. Most people tolerate it without issue. In fact, over 94% of people who go through this process end up being cleared of their allergy label. 3. Blood Tests (IgE Tests)
These exist, but they’re not very reliable. They’re good at ruling out allergies when positive (specificity is 95-98%), but they miss most true allergies (sensitivity is only 40-60%). So they’re not used alone. They’re a backup, not a replacement. The best approach? Skin test + oral challenge. It’s the gold standard. And it’s safe. In studies across U.S. hospitals, serious reactions during testing happened in less than 2% of cases-and almost all were mild.
Who Can Do the Testing?
You don’t need to see a specialist in a big city. More and more primary care doctors, pharmacists, and nurses are trained to do this. The American Academy of Allergy, Asthma & Immunology says non-allergists can safely perform de-labeling for low-risk patients after a short training period. At the University of Pennsylvania, nurses and pharmacists ran a penicillin de-labeling program that cleared over 1,800 patients between 2020 and 2023-with zero severe reactions. At Mayo Clinic, patients get tested in a single visit. Some hospitals now use automated tools built into electronic health records that flag patients for testing based on their history. The biggest barrier? Access. In rural areas, there’s often just one allergist for every 500,000 people. But that’s changing. Telemedicine is now approved for low-risk cases. A Dutch study showed 897 patients successfully completed remote evaluations and oral challenges at home-with a 96% success rate and no emergencies.
What Happens After Testing?
If the test is negative? Your allergy label is removed. That’s it. No more warnings. No more avoiding penicillin, amoxicillin, or other beta-lactams. You can now get the best, safest, cheapest treatment for infections. But here’s the catch: the label doesn’t disappear automatically. You have to make sure your medical records are updated. Tell your doctor. Ask your pharmacist. Check your EHR portal. If your chart still says “Penicillin Allergy,” you’re still at risk. Some hospitals now document allergies at the drug level-like “allergic to amoxicillin,” not “allergic to penicillin.” That’s better, because not all penicillins react the same. But if you’re cleared, you need to make sure your record says “penicillin allergy ruled out” or “tolerated penicillin on challenge.”Real Stories: What People Experience
One patient from Houston, 68, had a penicillin label since childhood. She’d been treated for urinary tract infections with expensive, harsh antibiotics for decades. After testing at a local clinic, she was cleared. Within months, she took amoxicillin for a new infection-and had no reaction. Her next hospital bill was $28,500 lower than it would’ve been with the old drugs. Another Reddit user, “PenicillinCurious22,” had a rash at age 5. For 17 years, she avoided penicillin. She got Z-Paks instead-and they gave her terrible stomach pain. After a three-step challenge at Mayo Clinic, she was cleared. Now she takes amoxicillin without issue. “I didn’t realize how much I’d been suffering,” she wrote. But not everyone has a smooth experience. One patient on HealthUnlocked had a mild wheezing reaction during a direct challenge without skin testing. She was correctly labeled afterward-but says she wishes they’d done the skin test first. That’s why guidelines stress risk stratification: low-risk patients can skip skin testing. Moderate-risk patients shouldn’t.What’s Changing in 2026?
The system is finally catching up. In January 2024, the CDC launched the “Allergy Alert Initiative,” funding 12 regional centers to help safety-net hospitals implement testing. By 2026, they aim to cut false penicillin labels in half. Medicare and Medicaid are now tracking de-labeling as a quality metric. Hospitals that don’t reduce inappropriate antibiotic use in patients with penicillin labels could lose funding starting in 2025. And software companies like Epic are building tools that automatically suggest testing when a patient’s record shows a penicillin allergy. Since 2021, their system has helped remove 198,000 false labels across U.S. hospitals.
What You Should Do Now
If you’ve ever been told you’re allergic to penicillin-or any antibiotic-here’s what to do:- Look at your medical records. Does it say “penicillin allergy” without details? That’s a red flag.
- Ask yourself: What was the reaction? Was it a rash? Nausea? Diarrhea? Or hives, swelling, or trouble breathing?
- If it was a mild rash or side effect, you’re likely not allergic. Ask your doctor about testing.
- Request a referral to an allergist-or ask if your primary care provider offers de-labeling.
- If testing is available, get it done. It’s safe, fast, and free or low-cost in most cases.
- Once cleared, make sure your records are updated. Tell every doctor, pharmacist, and hospital you visit.
Common Questions About Drug Allergy Testing
Can I outgrow a penicillin allergy?
Yes. Most people who had a true penicillin allergy as children lose it over time. Even if you were allergic 10 or 20 years ago, you’re likely not anymore. Studies show that 80% of people who had a true IgE-mediated reaction lose sensitivity after 10 years. That’s why testing is recommended even for long-standing labels.
Is drug allergy testing painful?
Skin testing feels like a tiny pinch-similar to a blood draw. Oral challenges involve swallowing pills or liquid. Most people feel nothing. If you’re nervous, ask for a numbing spray before skin testing. The process is designed to be as comfortable as possible.
What if I have a reaction during testing?
Testing is done in controlled settings with emergency equipment on hand. If you react, the team will stop the test and treat you immediately. Reactions are rare-and almost always mild. Even if you do react, you’ll get a correct diagnosis. That’s better than living with a false label.
Can I be allergic to one penicillin but not another?
Yes. Penicillin is a class of drugs. Amoxicillin, ampicillin, and cephalexin are all related, but cross-reactivity isn’t guaranteed. Someone allergic to amoxicillin might tolerate cephalexin. That’s why testing is done with the specific drug you need-not just “penicillin.”
How long does the testing take?
Skin testing takes about 30 minutes. The oral challenge adds another 1 to 2 hours. Most people complete everything in a single visit. Some clinics offer split visits if you prefer. There’s no need to take days off work.
Is testing covered by insurance?
Yes. Most insurance plans, including Medicare and Medicaid, cover allergy testing for drug reactions. The cost of testing is far less than the cost of an unnecessary hospital stay or a course of a more expensive antibiotic. Ask your provider for pre-authorization if needed.

So I got labeled allergic to penicillin when I was six after a rash from amoxicillin-turned out it was just heat rash from running around in a fever. I never questioned it for 30 years. Last year, I finally got tested at my local pharmacy clinic. They did the skin prick, then gave me a tiny pill. No reaction. No drama. Just… freedom. Now I take amoxicillin for every UTI and sinus infection. My bills dropped, my stomach stopped hating me, and honestly? I feel like I got my health back. Why don’t more people know this exists?
It is imperative to underscore the clinical and public health significance of this issue. The persistence of inaccurate penicillin allergy labels constitutes a systemic failure in medical documentation and patient education. Evidence-based de-labeling protocols, when implemented with fidelity, demonstrably reduce antimicrobial resistance, lower healthcare expenditures, and improve patient outcomes. The integration of standardized screening tools into electronic health records represents a critical step toward institutional accountability and patient safety.
Think about it-our entire medical system is built on mythic narratives passed down like family recipes. ‘Mom said I’m allergic.’ ‘The nurse wrote it down.’ ‘I felt weird once.’ We treat drug allergies like astrology: vague, emotional, and completely detached from biology. Meanwhile, real science-skin tests, oral challenges, IgE quantification-is sitting in labs, waiting for the public to stop treating their medical records like a haunted diary. We’re not just misusing antibiotics-we’re misusing our own bodies, haunted by ghosts of childhood rashes. Wake up. The immune system doesn’t hold grudges. The system does.
They’re hiding the truth. Big Pharma doesn’t want you to know you can get tested. Why? Because those ‘alternative’ antibiotics? They’re more profitable. The CDC? They’re funded by the same companies pushing those drugs. They’re not fixing the problem-they’re rebranding it as ‘awareness.’ You think they’d let you save money and get better care? Nah. They want you dependent. Stay woke. This isn’t medicine. It’s a money trap.
Bro this is wild. In India, we don’t even have access to proper testing. Most doctors just write ‘allergy’ because they don’t want to deal with it. I had a cousin who got a rash after amoxicillin at 8 and now at 32 she can’t take any beta-lactams. Her last pneumonia cost 3x more than it should’ve. We need to push for this here too. Maybe telemedicine can help? I saw a video of someone doing the challenge at home in the Netherlands. If they can do it, why not us?
I’ve been avoiding penicillin since I was 5. Never had a real reaction. Just a rash. But I never asked. I just accepted it. Now I’m wondering how many other things I’ve been avoiding because I was told to. What else am I misinformed about? This feels like a domino effect.
Oh, so now we’re supposed to trust ‘pharmacists’ and ‘nurses’ to perform life-altering medical tests? Who authorized this? Where’s the oversight? The CDC? The AMA? Where’s the board certification? This is reckless. You don’t just ‘clear’ a drug allergy like you’re deleting a spam email. People die from anaphylaxis. And now you want to hand this over to someone who took a 3-hour online course? This isn’t progress. It’s negligence dressed up as innovation.
How many people, after being cleared of a penicillin allergy, go back to their doctor and say, ‘So… can you update my chart?’ Spoiler: almost none. Because bureaucracy is a religion, and the label is its sacred text. The test is free. The update? That’s where the real cost begins. And the system? It’s designed to make you give up. Brilliant, really.
This is why we need to stop being so careless with our health. People get rashes and think they’re allergic. Then they pass it on like a curse. Your kid gets labeled, then their kid gets labeled. And you wonder why antibiotics don’t work anymore. It’s not the bacteria. It’s the laziness. You didn’t suffer. You didn’t get tested. You just accepted the label. Now the whole country is paying for your ignorance.
This is such a good reminder that we don’t have to live with old labels. I used to think if something was written in my chart, it was forever. But now I see-our bodies change. Our knowledge changes. Why shouldn’t our records? If you’ve been avoiding penicillin for years and never had a real reaction, don’t wait. Ask. Get tested. It’s not risky-it’s empowering. You’ve got nothing to lose but a myth.
Let me guess-this is part of the ‘digital health’ agenda. Epic’s software is pushing this because they want to cut costs, not because they care about you. They’re removing labels to reduce liability, not to improve care. And once your allergy is ‘cleared,’ what happens if you have a delayed reaction years later? Who’s liable then? The pharmacist? The EHR vendor? The system is designed to shift blame, not fix problems.
I’m 42 and had a penicillin label since I was 4. My mom said I broke out in hives after a shot. I never questioned it. Last year I got a UTI, and my doctor asked if I’d ever been tested. I said no. She scheduled me for skin testing the next day. Negative. I took amoxicillin the next week. Zero reaction. I cried in the pharmacy parking lot. I spent 38 years being afraid of a ghost. Thank you for writing this.
Let’s be real-this is just another way to get people to trust the system more. ‘Oh, just get tested, it’s safe!’ But what if the test fails? What if the ‘safe’ oral challenge triggers a reaction? You’re still stuck with the label. And if you die? The hospital says ‘you were high-risk.’ The system protects itself, not you. This isn’t science. It’s PR with a stethoscope.
I’m a nurse and we’ve been doing this in our clinic for two years. We screen patients during check-ins. If they say ‘allergic to penicillin’ with no details, we ask: ‘What happened?’ 90% of the time, it’s a rash or nausea. We refer them to the pharmacist for a 20-minute test. Most people walk out cleared. The best part? They come back and thank us. Not because they saved money. Because they finally feel like they’re not broken.