When a doctor calls out a medication order over the phone or in a busy ER, lives hang in the balance. Verbal prescriptions aren’t just a convenience-they’re often a necessity. But they’re also one of the most dangerous moments in patient care. A single misheard word can mean the difference between healing and harm. In 2025, despite all the advances in electronic systems, verbal prescriptions still make up 10-15% of medication orders in hospitals and up to 25% in clinics. And the errors? They’re not rare. They’re predictable.
Why Verbal Prescriptions Are Still Necessary
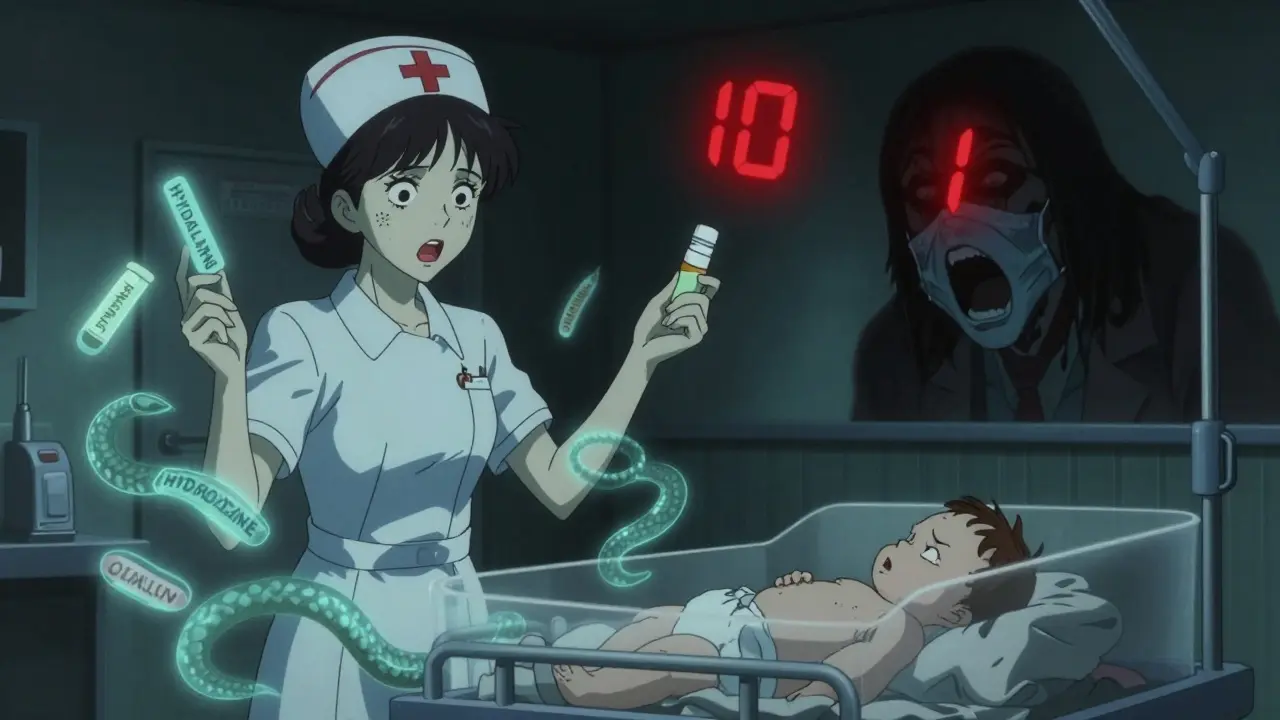
You might think we’d have eliminated verbal orders by now. After all, electronic prescribing cuts errors by up to 90%. But in real-world medicine, technology doesn’t always keep up with urgency. Surgeons operating in sterile fields can’t pull out tablets. Paramedics en route to the hospital need to order epinephrine before arrival. A nurse in the NICU might need to confirm a dose while holding a trembling newborn. These aren’t edge cases-they’re daily realities. The Institute for Safe Medication Practices says it plainly: “The only real record of a verbal order is in the memories of those involved.” That’s terrifying when you consider how easily memories fail. A 2021 Medscape survey found 68% of nurses had at least one near-miss every month due to unclear speech. Sometimes it’s a mumbled “fifteen” instead of “five.” Other times, it’s “Hydralazine” mistaken for “Hydroxyzine”-two drugs with wildly different effects. One lowers blood pressure. The other treats anxiety. Give the wrong one to a premature infant, and the result can be fatal.The Core Rules: What Every Provider Must Do
There’s no magic trick to making verbal prescriptions safe. Just discipline. And a few non-negotiable steps that every clinician, nurse, and pharmacist must follow-every single time.- Read-back is mandatory. The person receiving the order must repeat it back word-for-word. Not “I think it was ampicillin, 200 mg.” Not “Was it once or twice a day?” Full repetition: “Ampicillin, spelled A-M-P-I-C-I-L-L-I-N, two hundred milligrams, intravenous, every six hours, for suspected sepsis. Prescribed by Dr. Patel.”
- Spell everything phonetically. Never say “Zyprexa.” Say “Z-Y-P-R-E-X-A.” Never say “Celexa.” Say “C-E-L-E-X-A.” Sound-alike drugs like Celebrex and Celexa, Zyrtec and Zyprexa, have caused dozens of documented deaths. Spelling it out removes ambiguity.
- State numbers twice. Say “fifteen milligrams,” then “one-five milligrams.” This prevents confusion between 15 and 5, or 50 and 5. In high-stakes settings, this single step has prevented overdoses.
- Avoid all abbreviations. No “BID,” no “QID,” no “PO,” no “IV.” Say “twice daily,” “four times daily,” “by mouth,” “intravenous.” Abbreviations are the #1 source of misinterpretation.
- Never give multiple orders at once. One drug. One dose. One route. One frequency. Period. Trying to rush through three orders during a shift change? That’s how a baby gets the wrong antibiotic. The Pennsylvania Patient Safety Authority documented this exact error in 2006-and it still happens.
High-Risk Medications: When Verbal Orders Are Forbidden
Not all drugs should ever be ordered verbally. Some are too dangerous. The Pennsylvania Patient Safety Authority and the Washington State Department of Health both prohibit verbal orders for chemotherapy unless it’s to hold or stop treatment. Insulin, heparin, and opioids? Same rule. In non-emergencies, these must be ordered electronically or via written form. Why? Because the margin for error is microscopic. A 10-fold overdose of insulin? That’s not a mistake-it’s a death sentence. A nurse in Bristol told me about a case where a patient received 10 units of insulin instead of 1 because the prescriber said “ten” without spelling it out. The patient went into a coma. They survived, but only because the nurse double-checked the chart. Even in emergencies, the rules tighten. If you must give a verbal order for an opioid, you must state the exact dose, route, and indication. And you must document it within 30 minutes-not two hours, not the next shift. Johns Hopkins requires authentication by the end of the same shift. No exceptions.
Who’s Responsible? Everyone.
This isn’t just the doctor’s job. It’s the nurse’s. The pharmacist’s. The unit clerk’s. A 2020 Joint Commission survey found 63% of nurses said some prescribers refuse to accept read-backs. “It’s too slow,” they say. “I’m busy.” But safety isn’t optional. When a nurse skips the read-back because “I know what he meant,” that’s not experience-that’s recklessness. The American Nurses Association’s 2022 survey showed 87% of nurses support mandatory read-back protocols. Yet only 58% say they’re consistently followed in their unit. Why? Pressure. Burnout. Poor training. One ER nurse told me: “I’ve had to remind five different doctors this week to spell out drug names. One of them got mad. But I’d rather get yelled at than bury a patient.”Documentation: The Only Permanent Record
A verbal order isn’t official until it’s written down. And not just scribbled on a sticky note. It must be entered directly into the electronic health record with:- Patient’s full name and date of birth
- Medication name spelled out
- Dose with units (e.g., “5 milligrams,” not “5 mg”)
- Route (intravenous, oral, subcutaneous)
- Frequency (twice daily, every 8 hours)
- Indication (e.g., “for acute pain,” “for atrial fibrillation”)
- Name and credentials of the prescriber
- Exact time and date the order was received
- Exact time and date the order was authenticated

What Happens When You Skip the Steps?
The 2006 NICU case is still taught in medical schools. A premature infant was being transferred. The on-call doctor gave a verbal order for two antibiotics: ampicillin 200 mg and gentamicin 5 mg, both IV. The nurse wrote down “ampicillin 200 mg IV” and “gentamicin 5 mg IV.” But the doctor had meant 20 mg of gentamicin. The nurse didn’t ask for clarification. The baby got five times the correct dose. Within hours, the infant developed kidney failure. They survived-but with permanent damage. That’s not an outlier. A 2023 ECRI Institute report found that 42% of verbal order errors happen during shift changes. That’s when fatigue hits. When handoffs are rushed. When someone says, “I’ll get to it later.”What’s Changing? And What’s Next
The good news? Verbal orders are declining. In 2006, they made up 22% of hospital orders. Today, it’s 10-15%. Why? CPOE systems. Voice-to-text tech. Better EHR integration. KLAS Research predicts by 2025, they’ll drop to 5-8%. But here’s the truth: they’ll never disappear. Not while we have trauma bays, operating rooms, and ambulances. Dr. Robert Wachter wrote in NEJM Catalyst in 2023: “Certain clinical scenarios will always require verbal communication, making safety protocols permanently necessary.” The FDA is now working on standardizing how high-risk drug names are pronounced. ISMP Canada’s 2020 guidelines are becoming national policy. Forty-two states now require read-back verification by law. That’s progress.Final Rule: When in Doubt, Stop
The most powerful tool in verbal prescribing isn’t a checklist. It’s a mindset. If something doesn’t sound right-stop. Ask again. Spell it. Confirm. Don’t be embarrassed. Don’t assume. Don’t rush. One nurse in a Reddit thread summed it up: “I once stopped a 10-fold hydralazine error because I asked, ‘Did you mean H-Y-D-R-A-L-A-Z-I-N-E?’ The doctor said yes. Then he paused. ‘Wait… I meant hydroxyzine.’ We caught it. He thanked me. I didn’t get a medal. But the patient went home.” Verbal prescriptions aren’t going away. But the mistakes? They’re preventable. Every time you follow the rules, you’re not just following protocol. You’re saving a life.Are verbal prescriptions still legal in 2025?
Yes, verbal prescriptions are still legal under CMS and The Joint Commission regulations as of 2025. However, they must follow strict safety protocols, including mandatory read-back verification and immediate documentation. Many states have incorporated these standards into licensure requirements, making compliance not just best practice-it’s the law.
What’s the most common cause of verbal prescription errors?
The most common cause is sound-alike drug name confusion. Examples include Celebrex and Celexa, Zyprexa and Zyrtec, and Hydralazine and Hydroxyzine. These pairs sound nearly identical when spoken, especially in noisy environments. The Institute for Safe Medication Practices reports that 34% of verbal order errors stem from this issue. Always spell drug names phonetically to prevent them.
Can nurses accept verbal orders from non-physicians?
It depends on state law and institutional policy. In most cases, only licensed prescribers-physicians, nurse practitioners, and physician assistants-are authorized to give verbal orders. Nurses should never accept orders from unlicensed staff, even if they’re told to. Always verify the prescriber’s credentials before proceeding.
Why is read-back so important?
Read-back is the only reliable way to confirm that the order was heard correctly. Human memory is fallible, especially under stress. Studies show that when read-back is used properly, medication errors drop by up to 50%. Skipping it is like skipping a seatbelt-you might get lucky, but the risk isn’t worth it.
What should I do if a provider refuses to use read-back?
Politely but firmly insist. Say: “I need to confirm the order with you for patient safety.” If they push back, document the interaction and notify your supervisor or safety officer. Many hospitals have anonymous reporting systems for safety concerns. Your job isn’t to be polite-it’s to protect the patient.
Are there any medications that should never be ordered verbally?
Yes. Chemotherapy, insulin, heparin, and opioids should almost never be ordered verbally outside of true emergencies. Even then, they require extra verification. The Pennsylvania Patient Safety Authority and Washington State Department of Health explicitly prohibit verbal orders for these drugs unless it’s to hold or discontinue treatment. Always check your facility’s high-alert medication policy.
How long do I have to document a verbal order?
CMS requires authentication within 48 hours. But best practice-and the standard at top hospitals-is to document it immediately, ideally before the shift ends. Delayed documentation increases the chance of miscommunication, forgotten details, or someone else acting on an unverified order.
Can I use abbreviations like “BID” or “IV” in verbal orders?
No. Never. The Institute for Safe Medication Practices and The Joint Commission ban all abbreviations in verbal orders. Say “twice daily” instead of “BID,” “intravenous” instead of “IV,” and “by mouth” instead of “PO.” Abbreviations are a leading cause of misinterpretation and have led to multiple patient deaths.

So if a doc says 'five' but means 'fifteen', we just gotta guess? That's wild. I get spelling stuff out but why not just use a simple app that reads it back to them? Like, why are we still doing this by ear in 2025?
i just had a nurse spell out 'hydralazine' last week and i thought she was being extra… then i found out the doc meant hydroxyzine. i almost cried. we got lucky.
the fact that we still have to spell out drug names like we're in a spy movie is either tragic or hilarious. pick one.
in my village back home, the herbalist never writes anything down. he whispers the remedy to the child's mother, and she remembers. we don't have EHRs, but we have trust. here, we have technology and zero trust. something's broken.
read-back is non-negotiable but nobody ever does it right. i once heard 'celexa' said like 'selexa' and no one caught it. i had to scream it was a drug not a brand of headphones
as a nurse from a mixed background, i’ve had docs say 'BID' like it's a secret handshake. i always reply 'twice a day' just to make sure. sometimes they roll their eyes. i don't care. i've seen what happens when you assume.
if you're too busy to spell out a drug name, maybe you're too busy to be prescribing.
the government is forcing us to do this because they don't trust doctors. but what about the nurses who lie about read-backs? we need cameras in every ER room, not more paperwork.
i've been training new interns on this for years. the ones who get it? they become the best clinicians. the ones who roll their eyes? they're the ones who get investigated later.
in india we say 'dose double check' even if it's obvious. it's not about distrust-it's about respect. for the patient, for the job, for the life. 🙏
if you don't follow these rules, you don't deserve to hold a stethoscope. period. no excuses. no 'i'm tired.' people die because of laziness.
it's funny… we have AI that can predict heart attacks, but we still rely on a nurse’s memory to catch a misheard 'ten' vs. 'one'. we've solved the impossible… and left the simple broken.
you know who's really behind this? Big Pharma. They want us to spell out names so we can't confuse their drugs with generics. they profit from confusion. i'm not paranoid. i've seen the emails.
every time i hear someone say 'it's just a verbal order' i want to scream. this isn't a coffee order. this is someone's heartbeat. if you're too tired to spell 'Hydralazine', then go home. your patient doesn't care about your burnout. they just want to live.