Cardiac Monitoring: What It Is, How It Works, and What You Need to Know
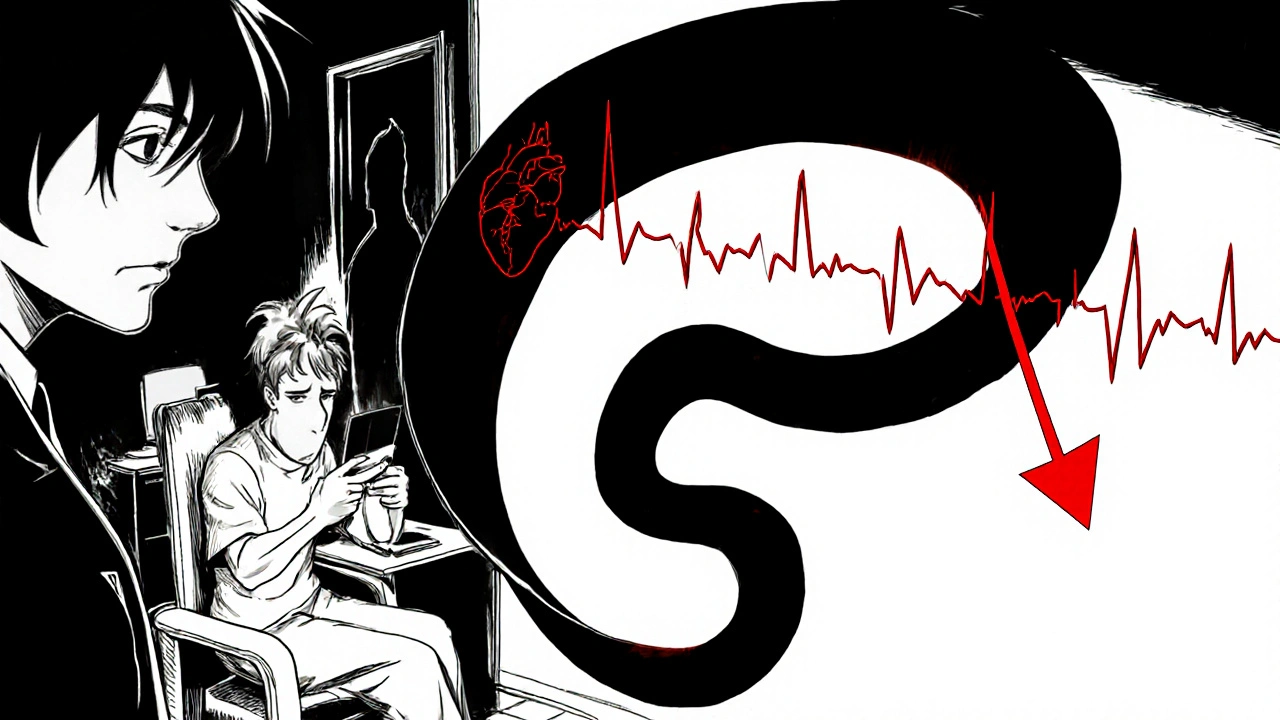
When your heart doesn’t beat right, it’s not always obvious—until something goes wrong. Cardiac monitoring, the continuous or intermittent tracking of heart activity to detect irregular rhythms and other issues. Also known as heart monitoring, it’s a simple, non-invasive way to catch problems like arrhythmia, atrial fibrillation, or silent heart damage before they become emergencies. You don’t need to feel dizzy or chest-tight to need it. Many people only find out they have an issue after a monitor picks up something their doctor missed during a quick checkup.
Cardiac monitoring isn’t just one thing. It includes everything from a quick ECG in a clinic to wearing a Holter monitor for 24 to 72 hours while you go about your day. Some devices even track your heart for weeks, sending data automatically to your doctor. These tools don’t just record beats—they show patterns. Is your heart skipping too often? Is it racing when you’re at rest? Is there a pause between beats that could mean trouble? That’s what these monitors reveal.
People with high blood pressure, a history of heart attacks, or unexplained fainting often get monitored. But it’s not just for the elderly. Young athletes with family histories of sudden cardiac events, people on certain medications like antidepressants or thyroid drugs, and even those with sleep apnea can benefit. If you’ve ever been told your heart "sounds funny" during a checkup, or if you feel your chest fluttering for no reason, cardiac monitoring might be the next step.
It’s not about fear. It’s about clarity. Most people who use these devices never find anything serious. But for those who do, catching it early can mean avoiding a hospital stay, a stroke, or worse. The data from these monitors helps doctors decide whether you need medication, a pacemaker, or just lifestyle changes. And sometimes, it’s the only way to prove that your symptoms are real—because heart problems don’t always show up on a standard test.
Below, you’ll find real, practical guides that break down how these devices work, what they can—and can’t—tell you, and how they connect to medications you might be taking. Whether you’re wondering if your palpitations are harmless or if your doctor’s recommendation makes sense, these posts give you the facts without the fluff.
Antipsychotics + QT‑Prolonging Drugs: How Combined Use Raises Arrhythmia Risk
Learn how antipsychotics combined with other QT‑prolonging drugs dramatically increase arrhythmia risk, and discover practical monitoring and drug‑selection strategies.
read more