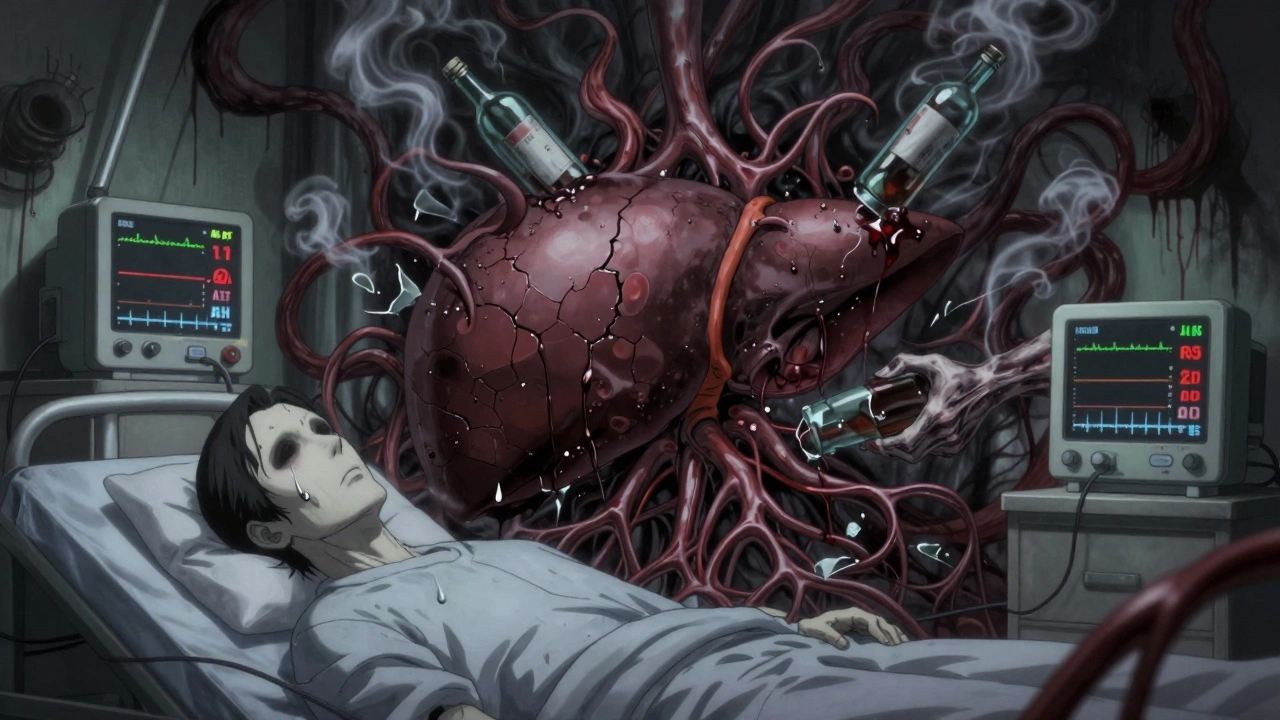
When someone stops drinking after years of heavy alcohol use, their body doesn’t just feel shaky-it’s in crisis. The liver, which has been working overtime to break down alcohol, suddenly has to reset. But this reset isn’t simple. Without the right support, stopping alcohol can actually make liver damage worse-even though the goal is healing.
What Happens to Your Liver When You Quit Drinking?
Your liver processes about 90% of the alcohol you consume. It turns ethanol into acetaldehyde, a toxic byproduct, then into acetate, which your body can use. But when you’ve been drinking heavily for months or years, this system gets overwhelmed. Fat builds up, inflammation spikes, and scar tissue starts forming. This is alcoholic liver disease (ALD), and it doesn’t just go away when you stop drinking.
Within hours of your last drink, your liver starts shifting gears. Blood flow changes. Enzymes go haywire. In fact, a 2002 study found that 32% of people who quit drinking saw their liver enzymes (AST and ALT) rise sharply in the first week-not because they drank more, but because the liver was under new stress. That’s right: stopping alcohol can temporarily make liver damage look worse on blood tests.
One key sign of alcohol-related liver damage is an AST:ALT ratio higher than 2:1. Normal is below 1:1. If your ratio is above that, it’s a red flag. Low albumin (under 3.5 g/dL) or a high INR (over 1.5) means your liver is struggling to make proteins or clot blood. These aren’t just numbers-they’re signals your liver needs help.
Why Medical Supervision Isn’t Optional
Trying to quit alcohol alone can be deadly. About 5% of people with severe alcohol dependence develop delirium tremens (DTs)-a life-threatening condition with confusion, seizures, and high fever. It usually hits 48-72 hours after the last drink. Without medical care, the risk of death from DTs is up to 35%. With supervision, it drops to under 5%.
Medically supervised detox uses benzodiazepines like chlordiazepoxide to calm the nervous system. These drugs aren’t just for anxiety-they prevent seizures and reduce brain overactivity caused by alcohol withdrawal. Studies show chlordiazepoxide is 85% effective at stopping seizures, while unmonitored symptom-based approaches only hit 40%.
And here’s the catch: hospitals and clinics don’t just manage symptoms. They protect your liver. That means checking your liver enzymes daily, giving you IV thiamine (500mg a day for 3-5 days) to prevent Wernicke-Korsakoff syndrome, and keeping you away from drugs that can poison your liver-even common ones like paracetamol (acetaminophen).
One study found that people who took just 1-2 grams of paracetamol a day during early withdrawal had the biggest spike in liver enzymes. That’s less than two standard painkillers. Your liver is so vulnerable right now that even normal doses become dangerous.
What Recovery Actually Looks Like
Recovery isn’t a single day or week. It’s a timeline.
- Days 1-3: Withdrawal peaks. Nausea, tremors, anxiety, and high blood pressure hit hard. Around 80% of people feel restless. About 75% can’t sleep.
- Days 4-7: Physical symptoms start to fade, but your liver is still in overdrive. This is when enzyme levels often peak. Medical teams monitor AST, ALT, and INR closely.
- Weeks 2-4: Liver enzymes begin to drop. If you had mild fatty liver, they may return to normal within 14 days. This is the first real sign your liver is healing.
- Months 2-4: Inflammation decreases. Fat starts clearing. If you had alcoholic hepatitis, this is when you see real improvement-if you’ve stayed sober.
- Months 6-12: Scar tissue stops forming. The liver begins to regenerate. Studies show that even after years of heavy drinking, the liver can recover significantly if you stop completely.
But here’s the hard truth: if you have cirrhosis, your liver can’t fully heal. Scar tissue stays. But stopping alcohol stops the damage from getting worse. That’s the difference between life and death.

What Actually Helps Your Liver Heal
Detox isn’t just about getting through withdrawal. It’s about giving your liver the tools to rebuild.
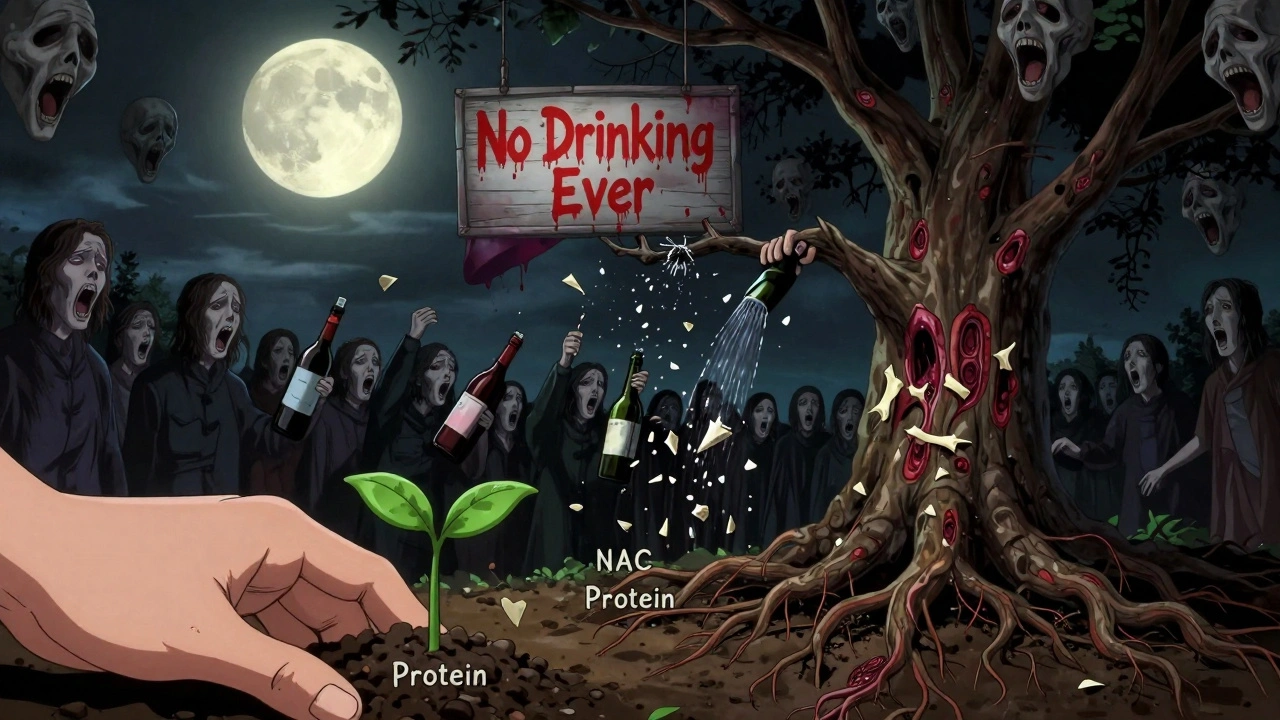
Nutrition is critical. Your body has been starved of vitamins and protein. A high-protein diet (1.2-1.5 grams per kilogram of body weight) helps repair liver cells. Think eggs, lean meats, beans, and dairy. Without enough protein, your liver can’t regenerate.
Vitamin B1 (thiamine) is non-negotiable. Alcohol depletes it. Low thiamine causes brain damage-Wernicke-Korsakoff syndrome. IV thiamine is given during detox because oral pills won’t absorb well when your gut is damaged.
N-acetylcysteine (NAC) is a supplement that helps your liver make glutathione, its main antioxidant. A 2021 trial showed NAC reduced liver enzyme spikes by 30% during withdrawal compared to placebo. It’s not magic, but it’s one of the few proven liver protectors during this fragile time.
Hydration and electrolytes matter too. Alcohol pulls water and minerals out of your body. Replacing sodium, potassium, and magnesium helps stabilize your heart and nerves.
And avoid everything else: no NSAIDs like ibuprofen, no herbal supplements (some are liver-toxic), no energy drinks, no “detox teas.” Your liver is already overloaded. Don’t add to it.
What Doesn’t Work-and Why
Some people try to quit slowly-cutting back over weeks. It sounds safer, but it’s risky. If you’re still drinking, even a little, your liver keeps getting damaged. A 2021 study found that 35% of people using tapering for moderate to severe dependence relapsed or kept harming their liver.
Home detox? Only 65% of people survive it safely. In a hospital or clinic, it’s 95%. Why? Because you need constant monitoring. Blood pressure spikes? Liver enzymes rising? Seizure risk? These can’t be handled over Zoom or by a friend.
And don’t believe the myth that “a little wine is okay now.” For anyone with liver damage, even one drink can restart inflammation. The NHS says: if you have alcoholic hepatitis or cirrhosis, you need lifelong abstinence. No exceptions.
Who’s at Risk-and Why Access Matters
Men make up 70% of cases. Most are between 45 and 65. But rates in women have jumped 40% since 2010. Why? Social norms changed. Marketing targeted women. Stress and isolation increased. Alcohol isn’t just a “man’s problem” anymore.
But help isn’t evenly available. Only 15% of rural areas in the U.S. have proper detox centers. Insurance coverage varies wildly-private insurance covers 85% of detox costs. Medicaid covers only 45%. That means people with lower incomes are more likely to try dangerous home detox.
And the cost of inaction? Alcohol-related liver disease kills 40% of all liver disease deaths in Western countries. It costs the U.S. healthcare system $29 billion a year. Most of those deaths are preventable-if people get the right help at the right time.
What Comes After Detox
Detox is just the first step. Seven out of ten people who finish detox but don’t get ongoing support relapse within six months. And if they drink again, all the liver recovery is undone.
Long-term success needs therapy, peer support, and sometimes medication like naltrexone or acamprosate. These aren’t “crutches”-they’re tools to rewire cravings.
For those with mild liver damage, a doctor might allow light drinking after six weeks of abstinence-no more than 14 units a week (about 6 pints of beer or 7 small glasses of wine). But if you’ve had hepatitis or cirrhosis? No drinking ever. That’s not a suggestion. It’s survival.
Future treatments are coming. Researchers are testing drugs that block fibrosis (like those targeting TIMP1). Some clinics now use real-time liver monitoring during detox to catch problems early. But none of that matters if you don’t get access to basic care.
The truth? Your liver is one of the most resilient organs in your body. It can heal-even after years of abuse-if you give it a real chance. But that chance only comes with safety, support, and science-not willpower alone.
Can you reverse liver damage from alcohol?
Yes, but only if you stop drinking completely. Fatty liver can reverse in weeks. Alcoholic hepatitis improves in months if you quit. But cirrhosis-the scarring-is permanent. Still, stopping alcohol stops further damage and can prevent liver failure. The liver regenerates cells, but it can’t undo scar tissue.
Is it safe to quit alcohol cold turkey at home?
No, especially if you’ve been drinking heavily for more than a few months. Withdrawal can cause seizures, delirium tremens, and even death. Medical supervision reduces death risk from 35% to under 5%. Even if you feel fine, your liver and brain are under stress. Don’t risk it.
Can you take painkillers like paracetamol during alcohol withdrawal?
Avoid paracetamol (acetaminophen) completely during withdrawal. Your liver is extra sensitive. Even a normal dose-like two 500mg tablets-can cause severe liver injury. Use acetaminophen-free pain relief only if approved by your doctor. Ibuprofen and other NSAIDs can also stress your kidneys and liver-so skip them too.
How long does it take for liver enzymes to return to normal?
In mild cases, AST and ALT levels start dropping within 7-14 days after quitting. Full normalization can take 4-8 weeks. But if you have advanced disease, enzymes may stay elevated longer. The key isn’t just the numbers-it’s staying sober. One drink can push them back up.
Do you need to be hospitalized for alcohol detox?
If you’ve been drinking heavily for over a year, have a history of seizures, or have liver disease, yes. Hospital or clinic detox is safest. You’ll get IV fluids, thiamine, medications to control withdrawal, and constant monitoring. Outpatient detox only works for mild cases-and even then, you need daily check-ins.
Can supplements like milk thistle help your liver during withdrawal?
There’s no strong evidence that milk thistle or other herbal supplements help during alcohol withdrawal. Some may even interact with medications or harm your liver. Stick to proven support: thiamine, NAC, protein, and medical care. Don’t gamble with your liver on unproven remedies.
What happens if you start drinking again after detox?
If you’ve had alcoholic hepatitis or cirrhosis, drinking again will speed up liver failure. Even if you had mild fatty liver, restarting alcohol restarts inflammation and fat buildup. Studies show 70% of people who relapse within six months lose all liver recovery progress. Sobriety isn’t a choice-it’s your only path to survival.

bro i quit drinking last year and my liver enzymes dropped like a rock 🤯 like 3 weeks in and my doc was like 'dude what did you do?' i didn't even take supplements just stopped cold turkey and ate eggs every day. liver is wild.
This post is accurate but the tone is too soft. People need to hear this: if you're still drinking to 'manage stress,' you're not healing-you're just delaying death.
NAC? Really? You're telling me to spend money on some supplement when the real fix is just not drinking? This is why people get scammed. Stop buying snake oil and start living.
I've been a nurse in detox for 12 years and I can tell you the #1 thing that saves lives isn't the meds-it's the damn thiamine. So many people come in with no B1 and their brains are basically frying. IV thiamine isn't optional. It's life support.
The AST:ALT ratio >2:1 is a classic marker, but it's often misinterpreted. In early withdrawal, AST spikes first because of muscle breakdown from tremors-not just hepatocyte damage. Always correlate with clinical presentation. Also, INR >1.5 is a red flag for synthetic failure. This isn't just 'liver stuff'-it's coagulopathy territory.
I read this and thought 'finally someone gets it' 😭 my dad died of cirrhosis at 58. He tried to quit at home. They said 'just drink water.' He lasted 72 hours. Then he had a seizure in the shower. No one knew what to do.
In India we dont have clinics for this so people use home remedies like neem juice and black salt and think they are fine. I saw a man die because he took paracetamol for headache during withdrawal. He thought it was just pain. Liver dont care what you think
I just read this because my boyfriend is trying to quit. Honestly I'm scared. I didn't know even one painkiller could kill him. I'm gonna delete all the tylenol in the house right now.
The resilience of the liver is one of the most profound biological phenomena. It operates on a principle of redundancy and regeneration that mirrors the Taoist concept of wu wei-effortless action. When we remove the obstruction (alcohol), the body's innate intelligence restores equilibrium. This isn't medicine-it's natural order.
I find it mildly amusing how this article frames sobriety as a 'scientific solution.' The truth is, no amount of NAC or IV thiamine can compensate for the moral failure of dependency. The real cure is discipline, not pharmacology. And if you need a hospital to stop drinking, perhaps you never truly wanted to.
Wait so if I had fatty liver and quit, can I drink again after 6 weeks? Like one beer? 🤔
No. Even one drink reactivates the inflammatory cascade in fatty liver. The window isn't a green light-it's a trap. The liver doesn't 'forgive' alcohol. The 14-unit limit only applies to those with zero prior damage. You're not one of them.
To all who are struggling: the path is hard but not impossible. You are not broken. You are becoming. Every day without alcohol is a victory. Your liver remembers your kindness. Keep going.
i quit 3 months ago and my skin looks better and i sleep like a baby 🙏 no more midnight snacks or rage crying. this post made me cry happy tears
This is the most comprehensive, clinically grounded, and humanely written piece on alcohol recovery I have ever encountered. It is not merely informative-it is a lifeline. I will be sharing this with every patient I counsel. The statistics are staggering, the science impeccable, and the compassion undeniable. Thank you.