Chronic kidney disease (CKD) doesn’t shout. It doesn’t cause pain or make you feel sick-until it’s too late. By the time symptoms like swelling, fatigue, or nausea show up, your kidneys may already be failing. But here’s the truth: CKD can be caught early, and when it is, progression can often be stopped. In the U.S., 1 in 7 adults has CKD. Most don’t know it. That’s not because they’re ignoring their health-it’s because routine checkups rarely include the right tests.
What Chronic Kidney Disease Really Means
CKD isn’t a single disease. It’s a label for long-term damage to your kidneys, lasting at least three months. This damage shows up in two ways: your kidneys can’t filter blood properly, or they leak protein into your urine. The key is that both things can happen long before you feel anything wrong.
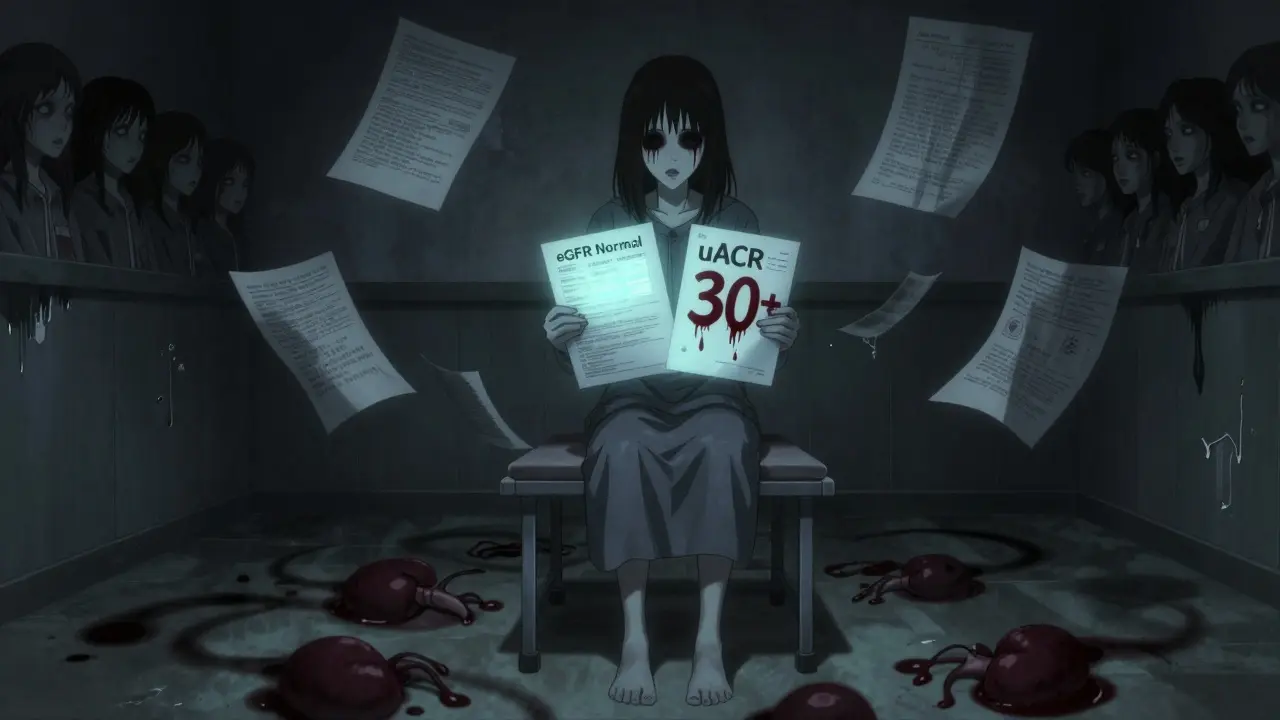
The standard way to measure kidney function is through eGFR-estimated glomerular filtration rate. It tells you how well your kidneys are filtering waste. A normal eGFR is above 90. If it drops below 60 for three months or more, that’s CKD. But here’s the catch: many people with early CKD have an eGFR above 60. Their kidneys still work well enough to keep them feeling fine. That’s why the second test matters more than you think.
The Two Tests That Save Kidneys
You need two tests to catch CKD early: eGFR and uACR. uACR stands for urine albumin-to-creatinine ratio. It measures how much protein (albumin) is leaking from your kidneys into your urine. A value of 30 mg/g or higher means damage is happening-even if your eGFR is normal.
For years, doctors relied only on eGFR, calculated from a blood test for creatinine. But creatinine levels change with muscle mass, age, diet, and even race. That means eGFR alone misses up to 40% of early CKD cases. A 2018 national survey found that people with diabetes or high blood pressure were being told their kidneys were fine, when they were already leaking protein. That’s how many people end up in dialysis without ever having warning signs.
That’s why guidelines from the National Kidney Foundation and KDIGO now say: both tests are required. One abnormal result isn’t enough. You need two abnormal tests, three months apart. That’s how you rule out temporary issues like dehydration or infection.
Stages of CKD: Why Early Matters
CKD is divided into five stages. Stage 1 and 2 are early. At these stages, your kidneys are still working, but damage is visible. Stage 1: eGFR ≥90 with protein in urine. Stage 2: eGFR 60-89 with protein in urine. These are the stages where intervention works best.
Stage 3a (eGFR 45-59) is where many people get diagnosed-often after years of undetected damage. Stage 3b and beyond mean serious decline. Stage 5 is kidney failure. At that point, your only options are dialysis or transplant. But if you catch it at stage 1 or 2, you have a 5- to 7-year window to slow or stop the damage.

Who Should Be Tested-and How Often
Not everyone needs regular kidney screening. But if you have any of these, you’re at risk:
- Diabetes (type 1 or 2)
- High blood pressure
- Family history of kidney failure
- Heart disease
- Obesity
- Being African American, Native American, or Hispanic
- Long-term use of NSAIDs like ibuprofen or naproxen
For people with diabetes, annual testing is mandatory. The American Diabetes Association says: test at diagnosis for type 2, and five years after diagnosis for type 1. For high blood pressure, check both eGFR and uACR at least once a year. If you’re over 60, ask your doctor. If you’re on multiple medications, ask again.
Black Americans are 3.7 times more likely to develop kidney failure than white Americans. That’s not genetic. It’s because they’re less likely to get screened. A 2021 CDC report showed that even when Black patients had diabetes or hypertension, they were 30% less likely to have their urine tested for protein.
What Happens When You Catch It Early
Early detection isn’t just about knowing the number. It’s about acting on it.
One study showed that people with stage 2 CKD who started taking an SGLT2 inhibitor (a class of diabetes drugs like dapagliflozin) cut their risk of kidney failure by 32%. Another study found that keeping blood pressure under 130/80 (instead of 140/90) reduced kidney decline by 27%.
But drugs aren’t the only answer. Dietary changes help. Reducing salt, avoiding processed foods, and controlling blood sugar can slow decline. A 2022 meta-analysis found that patients who got coaching on diet, medication, and lifestyle cut their rate of kidney function loss from 3.5 mL/min/year to just 1.2 mL/min/year. That’s a 66% improvement.
And it’s not just about the kidneys. CKD increases heart attack and stroke risk. When you treat early, you protect your heart, too.

Why So Many Cases Are Still Missed
Here’s the ugly truth: doctors aren’t always ordering both tests. A 2022 study in the Annals of Internal Medicine found that only 52.7% of primary care providers consistently ordered both eGFR and uACR for at-risk patients. In rural clinics, that number dropped to 31.7%.
Why? Electronic health records don’t always prompt for both. Many doctors still think creatinine is enough. Patients don’t ask. One Reddit user wrote: “My doctor checked creatinine for 10 years. When they finally did the urine test, I was stage 3.” Another said: “Caught at stage 1. Five years later, still stage 1. I changed my diet. Took my meds. I’m fine.”
There’s also a problem with overtesting. In elderly patients over 85 with mild eGFR drop (45-59) but no protein in urine, intervention often does more harm than good. Their kidneys may just be aging. That’s why guidelines stress: proteinuria must be present to confirm early CKD.
What’s Changing Now
The system is slowly fixing itself. In 2023, the FDA cleared the first AI tool-NephroSight by Renalytix-that predicts CKD risk using 32 data points before eGFR drops. It’s being tested in VA hospitals and could be in primary care by 2025.
Also, the Biden administration launched a $150 million program to make dual-testing mandatory in federally funded clinics by 2026. That’s expected to catch 1.2 million undiagnosed cases.
And the way eGFR is calculated is changing. For decades, race was factored into the formula, which lowered eGFR for Black patients-even if their kidneys were healthy. New formulas are dropping race adjustments. Early data shows this could increase early detection in Black patients by 12.3%.
Point-of-care uACR tests are also coming. These are like pregnancy tests for your kidneys-give a urine sample, get results in 10 minutes. The Veterans Health Administration saw a 40% rise in screening rates after using them.
What You Can Do Today
If you’re at risk:
- Ask your doctor for both an eGFR and a uACR test. Don’t accept one without the other.
- If your uACR is 30 or higher, even with normal eGFR, ask for a repeat test in 3 months.
- If you have diabetes or high blood pressure, insist on annual testing-even if you feel fine.
- Keep a copy of your results. Track them over time. A drop of 5 mL/min/year is a red flag.
- Ask about SGLT2 inhibitors if you have diabetes and protein in urine. They’re not just for blood sugar.
Don’t wait for symptoms. Kidneys don’t warn you. But the tests do.
Can you have chronic kidney disease without symptoms?
Yes. In fact, most people with early-stage CKD (stages 1-3) have no symptoms at all. Fatigue, swelling, or nausea only appear when kidney function is severely reduced. That’s why testing with eGFR and uACR is essential-even if you feel fine.
Is a blood test enough to check for kidney disease?
No. A blood test only measures eGFR, which estimates how well your kidneys filter waste. But it can miss early damage. Protein in the urine (measured by uACR) is often the first sign of kidney injury. Both tests together are needed for accurate diagnosis.
What does a uACR result of 30 mg/g mean?
A uACR of 30 mg/g or higher means your kidneys are leaking protein, which signals damage. This is called albuminuria and is a key marker for early chronic kidney disease, even if your eGFR is normal. It requires follow-up and management to prevent further decline.
Can lifestyle changes really slow kidney disease progression?
Yes. Controlling blood pressure, reducing salt and processed foods, managing blood sugar, and avoiding NSAIDs like ibuprofen can significantly slow kidney decline. Studies show that with proper lifestyle changes and medication, the rate of kidney function loss can drop by more than 60%.
Why do some people get diagnosed late even if they see a doctor regularly?
Many doctors still rely only on blood tests for creatinine and calculate eGFR. But this misses up to 40% of early cases because it doesn’t detect protein leakage. If your doctor hasn’t ordered a urine test (uACR), you’re not getting the full picture. Always ask for both tests if you’re at risk.
