Amoxicillin Diverticulitis Assessment Tool
Assess Your Diverticulitis Situation
This tool helps determine if amoxicillin might be appropriate for your diverticulitis treatment based on key clinical factors. Always consult with a healthcare provider before making treatment decisions.
Please fill out the form to see assessment results.
This tool provides general information only. It does not replace professional medical advice. Always consult a healthcare provider for diagnosis and treatment decisions.
Key Takeaways
- Diverticulitis is an inflammation of colon pouches that usually requires bowel rest and broad‑spectrum antibiotics.
- amoxicillin is not a first‑line choice, but it may work for mild cases without perforation when culture‑guided.
- Evidence from 2022‑2024 clinical trials shows mixed results; success depends on the bacteria involved.
- Common side effects include GI upset and rare allergic reactions; overuse can fuel antibiotic resistance.
- Talk to a healthcare provider before swapping standard regimens for amoxicillin.
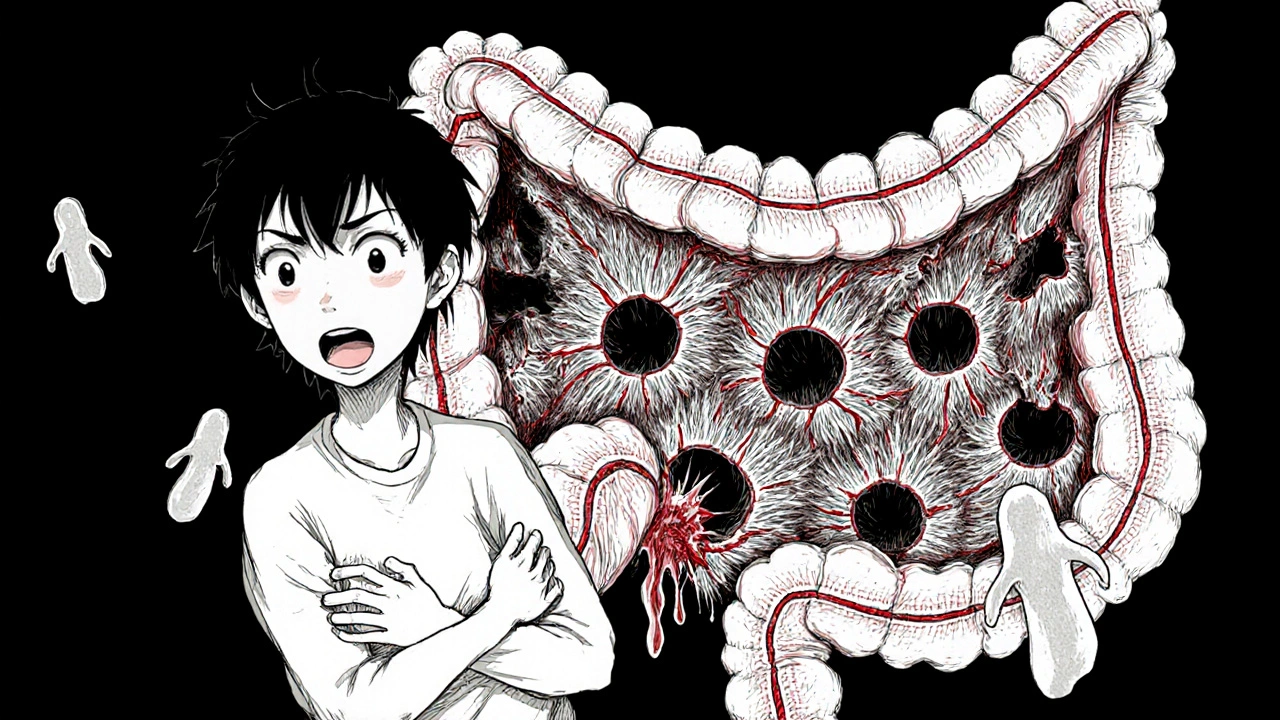
What Is Diverticulitis?
Diverticulitis occurs when tiny outpouchings (diverticula) that line the Colon develop inflammation or infection. It often presents with sudden abdominal pain, fever, and a change in bowel habits. In most cases the condition is sparked by micro‑tears that let gut bacteria seep into the diverticulum, triggering an immune response.
Standard Treatment Options
Guidelines from the American Gastroenterological Association (2023) recommend a stepped approach:
- Bowel rest: clear liquids for 24‑48 hours, then gradual reintroduction of low‑fiber foods.
- Broad‑spectrum antibiotics: typically a combination of Metronidazole (covers anaerobes) plus a fluoroquinolone like Ciprofloxacin (covers Gram‑negative organisms). For patients with contraindications to fluoroquinolones, a regimen of Trimethoprim‑sulfamethoxazole is often used.
- Imaging follow‑up: a CT scan after 48‑72 hours confirms response or flags complications.
Most uncomplicated cases improve within a week, and surgery is reserved for recurrent or perforated disease.
How Amoxicillin Works
Amoxicillin is a beta‑lactam antibiotic that blocks the synthesis of bacterial cell walls, leading to cell death. It is considered a narrow‑to‑moderate‑spectrum agent, effective against many Gram‑positive cocci (Streptococcus, Enterococcus) and some Gram‑negative rods (Escherichia coli, Haemophilus). Unlike fluoroquinolones, it does not reliably hit obligate anaerobes, which are common culprits in diverticular infections.
Evidence for Amoxicillin in Diverticulitis
Recent studies have explored amoxicillin as a single‑agent alternative:
- European Gastroenterology Trial (2022) - 120 patients with uncomplicated diverticulitis were randomized to amoxicillin + clavulanic acid versus standard metronidazole + ciprofloxacin. Clinical resolution at 7 days was 78 % for the amoxicillin arm versus 85 % for the standard arm (p = 0.12). The difference was not statistically significant, but adverse‑event rates were lower for amoxicillin.
- US Retrospective Cohort (2023) - 312 charts showed that physicians who used amoxicillin alone had a 10 % higher readmission rate for recurrent pain, suggesting gaps in anaerobic coverage.
- Canadian Microbiology Survey (2024) - Cultures from diverticular abscesses revealed 68 % anaerobes (Bacteroides fragilis group) and 32 % aerobic organisms. Amoxicillin alone would miss the majority of anaerobes.
Bottom line: amoxicillin may work for mild, early‑stage diverticulitis when the infection is dominated by susceptible aerobics, but it falls short for typical mixed flora.
When Amoxicillin Might Be Considered
Clinicians sometimes choose amoxicillin in the following scenarios:
- Patient has a documented allergy to fluoroquinolones and metronidazole.
- Local antibiogram shows low rates of anaerobic infection and high susceptibility of E. coli to amoxicillin.
- Cost or insurance barriers make the standard combo prohibitive; amoxicillin + clavulanic acid is a cheaper alternative.
- Early outpatient management of a small, localized flare where a short course (5 days) is planned.
In every case, treatment should be guided by stool cultures or, when feasible, percutaneous aspiration of the diverticular fluid for sensitivity testing.
Risks, Side Effects, and Antibiotic Resistance
Amoxicillin is generally well tolerated, but patients should watch for:
- Gastrointestinal upset - nausea, diarrhea, or abdominal cramping.
- Allergic reactions - rash, itching, or anaphylaxis in severe cases.
- Clostridioides difficile infection - a rare but serious consequence of any broad‑spectrum antibiotic.
- Development of resistant strains - overuse can breed beta‑lactamase‑producing E. coli, compromising future treatment options.
Balancing these risks against the modest benefit of amoxicillin is why it stays a secondary choice.
Practical Guidance: Dosage and Monitoring
If a clinician decides on amoxicillin, the typical regimen for an adult with diverticulitis is:
- Amoxicillin + clavulanic acid 875 mg/125 mg orally every 12 hours for 7‑10 days, or
- Amoxicillin 500 mg orally three times daily for 7 days (only if anaerobic coverage is deemed unnecessary).
Key monitoring points:
- Reassess pain and fever after 48 hours; lack of improvement warrants imaging.
- Check liver and kidney function if therapy exceeds 10 days.
- Educate patients about completing the full course, even if symptoms resolve early.
Comparison of Common Antibiotic Regimens
| Regimen | Spectrum | Typical Dose | Pros | Cons |
|---|---|---|---|---|
| Metronidazole + Ciprofloxacin | Anaerobes + Gram‑negatives | Metronidazole 500 mg q8h + Ciprofloxacin 500 mg q12h (7‑10 days) | Broad coverage, guideline‑backed | Fluoroquinolone side effects, drug interactions |
| Amoxicillin + Clavulanic Acid | Moderate aerobic + some anaerobes | 875 mg/125 mg PO q12h (7‑10 days) | Better tolerated, cheaper | May miss strict anaerobes, resistance risk |
| Trimethoprim‑Sulfamethoxazole | Gram‑negatives, some anaerobes | 800 mg/160 mg PO q12h (7‑10 days) | Alternative for fluoroquinolone allergy | Sulfa allergy, renal considerations |
Frequently Asked Questions
Can I self‑prescribe amoxicillin for diverticulitis?
No. Diagnosis and antibiotic choice should be made by a clinician who can assess severity, rule out complications, and choose the right drug based on local resistance patterns.
How long does a typical antibiotic course last?
Guidelines recommend 7‑10 days for uncomplicated cases. Shorter courses (<5 days) are being studied but aren’t standard yet.
What are the signs that antibiotics aren’t working?
Persistent fever, worsening pain, or new abdominal tenderness after 48 hours should trigger a repeat CT scan and possible change of antibiotics.
Is there a diet I should follow while on antibiotics?
Start with clear liquids, then move to low‑fiber foods for a few days. After the infection settles, a high‑fiber diet helps prevent recurrence.
Can probiotics reduce the risk of recurrence?
Some small trials suggest that a probiotic containing Lactobacillus acidophilus may lower recurrence, but evidence isn’t strong enough for a universal recommendation.
In sum, amoxicillin isn’t the go‑to drug for diverticulitis, but it can be a reasonable backup when allergies, cost, or local bacteria patterns line up. Always discuss options with a healthcare professional to avoid complications and to choose the safest, most effective regimen.

While the pathophysiology of diverticulitis hinges on transmural micro‑perforation, the selection of empiric antimicrobial coverage must reflect both aerobic and obligate anaerobic flora. Amoxicillin, despite its favorable safety profile, lacks sufficient activity against Bacteroides spp., which dominate the microbiome of diverticular abscesses. In scenarios where the local antibiogram demonstrates high susceptibility of Enterobacteriaceae to amoxicillin, it can be considered as a narrow‑spectrum adjunct. However, clinicians should remain assertive in ordering cultures before de‑escalating to a beta‑lactam monotherapy. Ultimately, the risk–benefit calculus should be guided by severity, comorbidities, and resistance trends.
Great rundown! 😊
The American Gastroenterological Association’s 2023 guideline remains the cornerstone for uncomplicated diverticulitis management.
The first‑line therapy typically combines a metronidazole‑based anaerobic agent with a fluoroquinolone to ensure broad coverage.
Amoxicillin, even when paired with clavulanic acid, falls short of this breadth because it does not reliably eradicate Bacteroides fragilis.
Multiple randomized trials between 2022‑2024 have explored amoxicillin as monotherapy, revealing modest success rates.
In the European Gastroenterology Trial, 78 % of patients achieved clinical resolution, compared with 85 % in the standard arm-a difference that failed to reach statistical significance.
Nevertheless, the amoxicillin arm demonstrated a lower incidence of Clostridioides difficile infection, highlighting a trade‑off between efficacy and safety.
The US retrospective cohort underscored a 10 % higher readmission rate when amoxicillin was used without anaerobic coverage, suggesting gaps in pathogen eradication.
When interpreting these data, it is crucial to consider the microbial landscape; about two‑thirds of diverticular abscess cultures are anaerobic.
Consequently, clinicians should reserve amoxicillin for patients with documented allergies to metronidazole or fluoroquinolones and who have favorable local susceptibility patterns.
Cost considerations also play a role, as amoxicillin‑clavulanate is often less expensive than a combination of metronidazole and ciprofloxacin.
However, insurance formularies increasingly favor the guideline‑recommended regimen, which can negate the price advantage.
Practical dosing for amoxicillin‑clavulanate is 875 mg/125 mg PO every 12 hours for 7‑10 days, with a caveat to monitor liver enzymes if treatment exceeds ten days.
Clinicians should reassess pain and fever at the 48‑hour mark; lack of improvement mandates repeat imaging to rule out complications.
Patient education is paramount-ensure they understand the necessity of completing the full course even if symptoms abate early.
In summary, while amoxicillin can be a viable alternative in select, low‑risk patients, it should not replace the guideline‑endorsed broad‑spectrum regimen for the majority of cases.
Looking at the data, it seems like amoxcillin could be a decent fallback when you cant use the usual combo. The key is to double‑check the local abitagram – if anaerobes are low, you might avoid a full‑spectrum shot. Still, don't forget to get culture results whenever possible, it helps tailor the therapy and kips resistance in check. Also, keep an eye out for any GI upset; it’s a common side effect you dont want to ignore.
Amoxicillin alone lacks anaerobic coverage; therefore, clinicians should be cautious.;
From a pathophysiological perspective, diverticulitis represents a micro‑environmental failure where mucosal integrity is breached, allowing a polymicrobial consortium to invade the submucosa. The therapeutic axis must therefore balance eradication of pathogenic flora with preservation of the commensal microbiome, a delicate ethical equilibrium. Amoxicillin, with its beta‑lactam core, offers a narrowed spectrum that aligns with the principle of antimicrobial stewardship, yet it may inadequately address obligate anaerobes that dominate the disease milieu. Consequently, its use embodies the philosophical tension between specificity and comprehensiveness, prompting clinicians to weigh the ontological certainty of culture‑directed therapy against the pragmatic urgency of empirical treatment. In practice, reserving amoxicillin for patients with documented allergies or favorable susceptibility profiles upholds both clinical efficacy and the broader societal imperative to mitigate resistance.
Think of the colon as a bustling kitchen; most dishes (bacteria) need a full pantry of spices (antibiotics) to keep the flavor balanced. Handing it just a slice of amoxicillin is like serving a plain bagel when the crowd craves a hearty sandwich-some will be satisfied, but many will leave hungry for the missing anaerobic “ingredients.”
While cost concerns are real, the guideline‑based regimen still provides the most reliable coverage for the typical mixed flora seen in diverticulitis. It’s important to discuss insurance options with patients early, so they aren’t surprised by out‑of‑pocket expenses later.
Oh sure, let’s just toss the standard combo out the window because “amoxicillin is cheaper.” As if the bacteria will magically care about our budget. Newsflash: you can’t win a war with a butter knife.
Everyone knows the pharma big guys push the fluoro‑quinolones so they can sell more pills. Amoxcillin is cheap, so they keep it quiet. Don't trust the guidelines, they are just a marketing ploy.
Remember, you’re not alone in navigating this treatment maze. If you have an allergy to the first‑line agents, bring that up with your doctor right away-there are safe alternatives. Keep a symptom diary; noting pain levels and fever spikes can help your clinician decide if the chosen antibiotic is working or if you need a re‑evaluation.
Totally got u, hope u feel better soon!
From a clinical standpoint, the choice of antibiotic should reflect both the microbiological profile of diverticulitis and the patient’s individual risk factors. Amoxicillin’s limited anaerobic activity makes it suboptimal for most cases, but it remains a viable option when contraindications to first‑line agents exist.
Patients must follow the prescribed regimen exactly; deviation can lead to treatment failure and promote resistant bacteria. If amoxicillin is chosen, ensure that culture data support its use and monitor the patient closely for any sign of worsening infection.