
When you see someone vaping on the street, it’s easy to assume it’s just a cleaner version of smoking. After all, no smoke, no ash, no smell. But what’s actually in that vapor-and what’s it doing to your lungs? The truth isn’t as simple as marketing claims suggest. Vaping isn’t harmless. It’s not even close. And the damage isn’t always obvious until it’s too late.
What’s Really in Vaping Aerosol?
E-cigarettes heat a liquid-usually made of propylene glycol, vegetable glycerin, nicotine, and flavorings-into an aerosol you breathe in. Sounds harmless? Think again. That vapor isn’t just water. A University of North Carolina study found that the very ingredients used to make e-liquids are toxic to lung cells. And the more chemicals added, the worse it gets. Flavorings like diacetyl, once used in microwave popcorn, are linked to a rare but serious lung disease called bronchiolitis obliterans-sometimes called "popcorn lung." Even though diacetyl is banned in many countries now, other harmful chemicals remain.
Research from the American Lung Association confirms that vaping aerosols contain dangerous substances like acetaldehyde, acrolein, and formaldehyde. These are known to cause lung irritation, inflammation, and long-term damage. You’re also breathing in heavy metals-nickel, tin, lead-leached from the device’s heating coils. And benzene, a chemical found in car exhaust, shows up in some vape liquids. These aren’t theoretical risks. They’re measurable toxins in every puff.
The Immediate Effects on Your Lungs
You don’t need years of vaping to see harm. Within weeks, many users report a persistent cough, shortness of breath during light activity, or chest tightness. These aren’t just "annoyances." They’re signs your airways are reacting to chemical irritation. A 2025 report from Lyracore tracked lung health in daily vapers and found that even people with no prior lung issues developed signs of airway inflammation within three months.
One study showed that vapers had higher levels of inflammatory markers in their lungs than non-users. This inflammation doesn’t just go away when you stop vaping. It can lead to chronic bronchitis, reduced lung capacity, and worsening asthma. The CDC warns that vaping can trigger asthma attacks and make bronchitis harder to recover from. If you’re already dealing with asthma or COPD, vaping makes it worse. Fast.
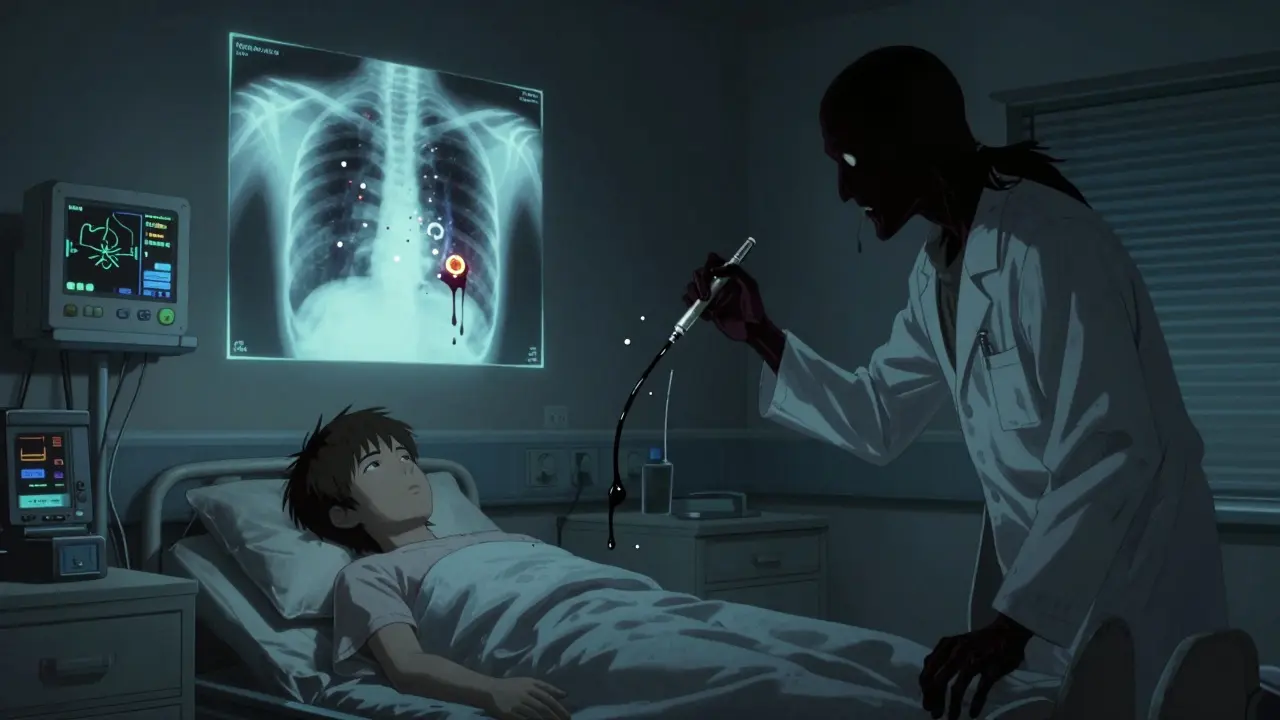
EVALI: The Outbreak That Changed Everything
In 2019, over 2,800 people in the U.S. were hospitalized with severe lung injury linked to vaping. Forty-seven died. This wasn’t a rumor. It was a public health emergency called EVALI-E-cigarette or Vaping Use-Associated Lung Injury. The cause? Vitamin E acetate, an additive used to thicken THC oil in black-market vape cartridges. It wasn’t nicotine. It wasn’t flavoring. It was a cutting agent that turned into a toxic goo when heated.
The scary part? EVALI could’ve been prevented. Regulators knew about the risks of unregulated additives, but enforcement was weak. The outbreak was a wake-up call: vaping products aren’t monitored like medicine. What’s in your cartridge? No one knows for sure unless you buy from a licensed, tested source-and even then, contamination is still possible.
Vaping and COPD: The Silent Threat
Chronic Obstructive Pulmonary Disease (COPD) used to be called a "smoker’s disease." But a 2024 NIH study analyzed data from over 40,000 adults and found that current e-cigarette users had a 48% higher risk of developing COPD than non-users. That’s not a small increase. That’s a clear, measurable danger. The study controlled for cigarette smoking, age, and other factors. The link held.
How does vaping cause COPD? It’s not the same as cigarette smoke. But the constant irritation from chemicals in aerosol damages the small airways and alveoli-the tiny sacs where oxygen enters your blood. Over time, this leads to scarring, loss of elasticity, and airflow blockage. Unlike smoking, where the damage builds over decades, vaping can accelerate this process in younger people who’ve never smoked before.
How Vaping Weakens Your Immune System
Your lungs have a built-in defense system. Special cells patrol the airways, trapping germs and clearing out debris. Vaping shuts down this system. Research from the American Thoracic Society found that e-cigarette vapor reduces the activity of immune cells in the lungs by up to 40%. That means you’re more likely to catch pneumonia, bronchitis, or even the flu.
One study showed that vapers had slower recovery times from respiratory infections. Another found higher rates of hospitalization for lung infections among young adults who vaped regularly. This isn’t about being "sick"-it’s about your body being less able to fight off what’s already out there. For teens and young adults, this is especially dangerous. Their immune systems are still developing. Vaping doesn’t just hurt lungs-it makes them vulnerable.

Is Vaping Better Than Smoking?
Yes, if you’re a current smoker switching completely to vaping, you’re likely reducing your exposure to tar and thousands of cancer-causing chemicals in tobacco smoke. That’s why some health groups support vaping as a harm reduction tool. But here’s the catch: "less harmful" doesn’t mean "safe." And for people who never smoked? There’s zero benefit.
Our World in Data estimates vaping is about 50-70% less harmful than smoking-but still carries significant risks. The problem? Many people, especially teens, think vaping is harmless. A 2025 survey found that 62% of high school vapers believed it had "no long-term health effects." That’s dangerously wrong. You can’t compare vaping to smoking like apples and oranges. They’re two different threats. Smoking kills slowly. Vaping damages quickly.
Who’s Most at Risk?
It’s not just long-term users. The biggest growth in vaping is among people under 30 who’ve never smoked. That’s a red flag. These are young lungs, still developing. The National Academies of Science found that teens who vape are more likely to develop coughing, wheezing, and asthma flare-ups. And once they’re addicted to nicotine, they’re more likely to start smoking cigarettes later.
People with pre-existing lung conditions-asthma, bronchitis, emphysema-are at even higher risk. Even occasional vaping can trigger attacks. And while older adults might think vaping is a safer alternative to quitting smoking, the evidence shows it doesn’t help much. Dr. NeSmith, a pulmonologist in Houston, says: "I’ve had patients quit cigarettes only to start vaping. They think they’re winning. But their lung function didn’t improve. It just changed shape."
What Should You Do?
If you vape and have symptoms-cough, shortness of breath, chest pain, frequent infections-see a doctor. Don’t wait. Get a lung function test. Ask about inflammation markers. Don’t assume it’s "just a cold."
If you don’t vape but are curious, know this: nicotine is addictive. The flavors are designed to hook you. The industry spends billions to make vaping look cool. But your lungs don’t care about the flavor. They only care about what’s in the vapor.
If you’re trying to quit smoking, there are safer, proven methods: nicotine patches, gum, counseling, prescription meds. Vaping isn’t the answer. It’s a different kind of risk.
And if you’re under 25? The best choice is to never start. Your lungs are still growing. Don’t gamble with them.
Can vaping cause lung cancer?
There’s no direct evidence yet that vaping causes lung cancer, but that doesn’t mean it’s safe. The chemicals in vape aerosols-like formaldehyde and acrolein-are known carcinogens. Studies show they cause DNA damage in lung cells, which is the first step toward cancer. It takes decades for cancer to develop, so we won’t have clear answers for years. But the damage is happening now.
How long does it take for lungs to heal after quitting vaping?
Improvement starts within weeks. Inflammation begins to reduce after 2-4 weeks. Lung function can improve by 10-15% in 3 months. But some damage, like scarring or reduced cilia function, may be permanent. The sooner you quit, the better your chances. People who vape heavily for years may never fully recover.
Are nicotine-free vapes safe?
No. Even without nicotine, the base liquids (propylene glycol and vegetable glycerin) and flavorings are still toxic to lung tissue. Studies show that nicotine-free vapes still cause airway inflammation and immune suppression. The danger isn’t just from nicotine-it’s from what you’re inhaling.
Do vape manufacturers know these risks?
Yes. Internal documents from major vaping companies, revealed in lawsuits and congressional hearings, show they were aware of toxic chemicals in their products as early as 2015. But they didn’t warn consumers. Instead, they marketed flavors like mango and mint to teens. The industry prioritized growth over safety.
Is secondhand vape aerosol dangerous?
Yes. The U.S. Surgeon General confirmed in 2016 that secondhand vape aerosol contains nicotine, ultrafine particles, and toxic chemicals like formaldehyde. Children and people with asthma are especially vulnerable. There’s no safe level of exposure. Just because you can’t smell it doesn’t mean it’s harmless.
If you’ve been vaping and you’re worried about your lungs, don’t wait for symptoms to get worse. Talk to your doctor. Get tested. Your lungs can’t tell you they’re hurting until it’s too late. But you can act now.

Let’s cut through the noise: vaping aerosol isn’t water vapor. It’s a cocktail of propylene glycol, VG, flavor esters, and metal particulates from the coil. Studies show even nicotine-free devices induce oxidative stress in bronchial epithelial cells. The diacetyl ban? Half-measure. We’re now seeing pentanedione and 2,3-pentanedione in flavorings-same mechanism, same lung damage. You’re not just inhaling flavor. You’re inhaling a toxicant matrix with no regulatory oversight. And the CDC’s 2019 EVALI outbreak? That was the tip of the iceberg. Most users don’t even know what’s in their cartridges. The industry doesn’t have to disclose. And that’s the real crime.
Y’all are acting like vaping is the new asbestos. Look-I quit smoking two years ago and switched to vaping. My lung function improved. My cough disappeared. I’m not some lab rat. I’m a 34-year-old guy who didn’t want to die of emphysema. Yeah, there are risks. But let’s not pretend that vaping is as bad as smoking. It’s not. The data says it’s 50-70% less harmful. That’s not nothing. If you’re using it to quit, you’re doing better than 80% of smokers who try cold turkey.
so like… i read this and i’m like… wait. so the gov’t banned diacetyl but now we got pentanedione? and they’re like ‘oh it’s fine’? and then there’s the metal leaching? and the benzene? and the FDA? yeah right. they’re all in bed with big vape. i saw a video where a guy opened a pod and it was just… sludge. like, what the f. this isn’t science. it’s corporate theater. they’re selling addiction disguised as harm reduction. and teens? they’re the target. mint? mango? come on. this is a pyramid scheme with lungs as the currency.
It is a moral abomination that the American populace has been systematically misled by corporate entities masquerading as wellness advocates. The deliberate targeting of minors through flavor engineering constitutes a breach of the social contract. The fact that these products are sold without pharmaceutical-grade purity standards is not merely negligence-it is criminal malfeasance. One cannot ethically justify the normalization of inhalation-based intoxicants under the guise of harm reduction when the long-term pathophysiological consequences remain unquantified and unregulated. This is not innovation. It is exploitation dressed in sleek packaging.
Just to clarify a common misconception: the 48% increased COPD risk in vapers from the 2024 NIH study was adjusted for confounders like age, sex, BMI, and prior smoking history. The mechanism isn’t tar-it’s chronic airway epithelial injury from aldehydes and free radicals. Cilia beat frequency drops. Mucociliary clearance slows. That’s how you get recurrent infections and eventual fibrosis. And yes, nicotine-free vapes still do this. The base liquids are hydrophobic solvents that disrupt surfactant function. No nicotine needed. The damage is biophysical. This isn’t speculation. It’s in vitro and bronchoalveolar lavage data from Johns Hopkins and UChicago. If you vape daily, you’re essentially giving your lungs a low-grade chemical burn every time you inhale.
I’ve been vaping for 3 years. No cough, no issues. But I also got my lung function tested last year-FEV1 was 98%, FVC 96%. I’m 22, active, no asthma. I’m not saying it’s safe. I’m saying maybe it’s not as bad as everyone thinks? I mean, if I stopped today, would my lungs bounce back? What’s the real recovery timeline? Just curious.
you think this is about health? nah. this is about control. the FDA, the CDC, the AMA-they all got paid off by Big Pharma. nicotine patches cost $200 a month. vape pods? $5. who benefits? not you. they made smoking illegal in public places, then banned tobacco, now they’re trying to ban vaping so you HAVE to use their overpriced, underperforming quit-smoking drugs. and don’t even get me started on the vitamin E acetate scare. that was a black-market thing. it’s like blaming knives because someone got stabbed. this is a manufactured panic to push pharmaceutical monopolies. they don’t want you to have choices. they want you dependent.
oh wow. so vaping causes cancer? and lung damage? and immune suppression? and it’s all hidden by ‘flavors’? cool. so basically, the same people who told us ‘asbestos is fine’ and ‘lead paint is safe’ are now selling us ‘vapor is clean.’ next they’ll say secondhand smoke is just ‘aesthetic mist.’ i’m not surprised. corporations don’t care if you die. they care if you keep buying. and if you’re dumb enough to think mint flavor is harmless? well… you’re part of the profit margin. congrats.
Hey, I get it. People are scared. I’ve worked with teens who started vaping because they thought it was ‘cool’ or ‘harmless.’ But the real issue isn’t just the science-it’s the messaging. We’re not helping by scaring people into silence. We need honest, accessible info. Not fearmongering. Not corporate fear. Not ‘you’re dying’ headlines. We need: ‘Here’s what’s in it. Here’s what it does. Here’s how to quit if you want. Here’s where to get help.’ If we treat people like idiots, they’ll tune out. If we treat them like people, they might listen. Vaping isn’t a moral failure. It’s a public health gap. Let’s fix it with compassion, not outrage.
Look, I’ve been a respiratory therapist for 22 years. I’ve seen COPD, I’ve seen bronchiolitis, I’ve seen kids in ICU with EVALI. I’ve held the hands of parents whose 16-year-old couldn’t breathe because they thought ‘cloud chasing’ was a game. And let me tell you-no one wakes up one day and says, ‘I want to ruin my lungs.’ They get hooked on flavor, then nicotine, then they think they’re in control. But the truth? The lungs don’t lie. They don’t have a voice until they’re failing. And when they do? It’s too late. I’ve had patients quit smoking, start vaping, and then end up on oxygen five years later because their alveoli got coated in lipid-laden debris from the VG and flavor oils. It’s not a myth. It’s a slow-motion collapse. And the worst part? They never saw it coming. Because no one told them the truth. And now, they’re paying for it with every breath.
So here’s the thing. I’m Australian. We’ve got way stricter regulations here. All vape devices must be registered. All liquids must be lab-tested for contaminants. Flavor limits? 10% max for sweet flavors. No candy-like packaging. No marketing to under-18s. And guess what? Vaping rates among teens dropped 60% in three years. So yeah, the tech can be dangerous-but it’s the lack of oversight, not the device, that’s the problem. The US is basically letting the Wild West run loose. If we had the same rules as the EU or Australia, most of these risks would be cut in half. It’s not that vaping is inherently evil. It’s that we let corporations run the experiment on our kids. And now we’re all cleaning up the mess.
Actually, I think Camille’s right. Fear doesn’t work. I got off cigarettes because someone showed me data-not a horror story. I still vape, but I only buy from licensed dispensaries that post lab reports. No mystery flavors. No black-market pods. I check the ingredients. If it says ‘proprietary blend,’ I walk away. It’s not about being perfect. It’s about being informed. And yeah, I’d rather have a 50% risk than a 100% one. But I get it. For non-smokers? Don’t start. For smokers? Maybe it helps. But let’s stop pretending we have all the answers. We don’t. And that’s why we need better science-not more outrage.