Elderly Medication Risks: What Seniors and Families Need to Know
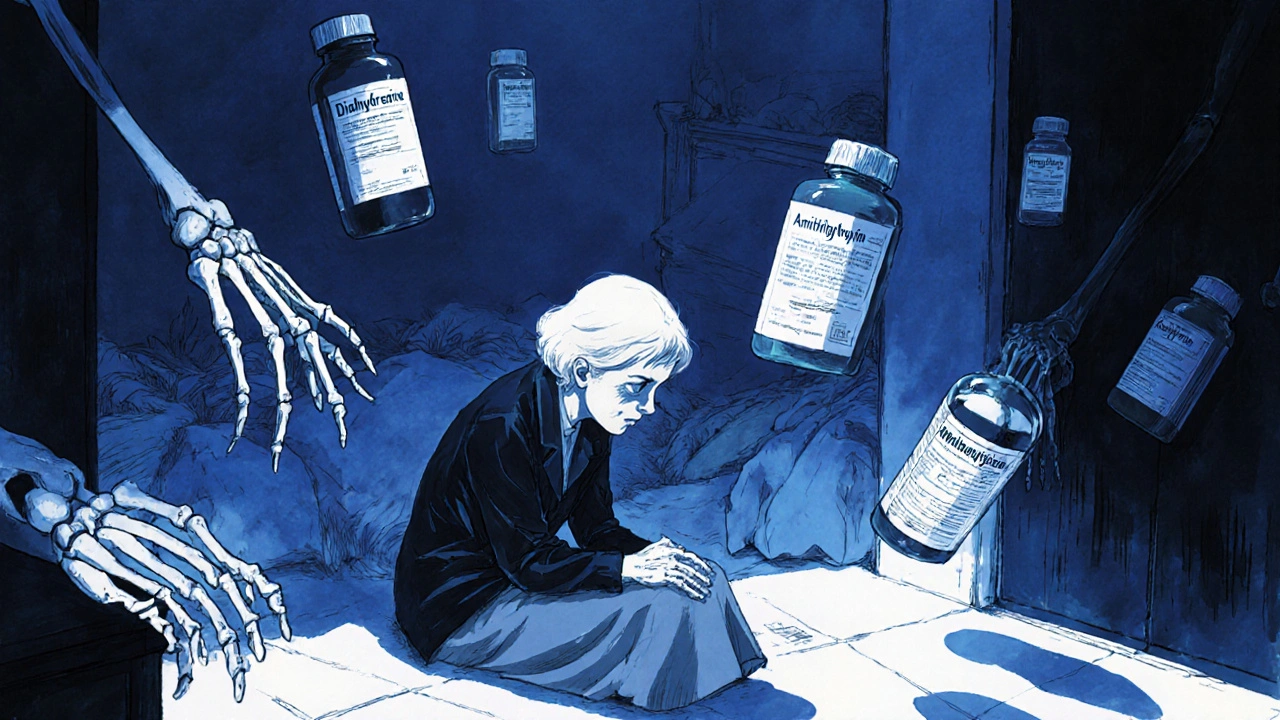
When someone over 65 takes multiple medications, they’re at higher risk for serious problems—elderly medication risks, the increased chance of harmful side effects, drug interactions, and dosing errors in older adults. Also known as polypharmacy dangers, this isn’t just about taking too many pills—it’s about how the body changes with age and how drugs behave differently in older systems. A 70-year-old with high blood pressure, arthritis, and sleep trouble might be on five or more prescriptions. Each one adds up. And what works fine for a 30-year-old can overload a 75-year-old’s liver, kidneys, or brain.
Polypharmacy, the use of multiple medications at once, often by older adults, is one of the biggest drivers of hospital visits in seniors. It’s not always the doctor’s fault—sometimes it’s because one specialist prescribes for heart issues, another for nerves, and another for pain, without seeing the full picture. And when pills look alike or labels get faded, confusion happens. Even over-the-counter sleep aids or antihistamines like dimenhydrinate, an antihistamine commonly used for motion sickness and allergies, Dramamine can cause dizziness, falls, or confusion in the elderly. Then there’s drug interactions in seniors, when two or more medications react badly together, often with life-threatening results. Think clarithromycin raising statin levels, or antidepressants mixing with blood thinners. These aren’t rare. They’re predictable—and preventable.
Age changes how the body handles drugs. The liver slows down. Kidneys filter less. Fat increases, water decreases. That means a standard dose of a sedative or painkiller might stay in the system twice as long. That’s why age-related drug metabolism, how the body processes and clears medications differently as people grow older matters more than the drug name itself. A pill that’s safe at 50 can be dangerous at 80. And many doctors still use the same dosing guidelines they learned in med school—guidelines that don’t account for these changes.
What you’ll find here aren’t theory-heavy articles. These are real, practical breakdowns of what goes wrong—and how to fix it. From understanding why generic drugs can still cause problems in older adults, to spotting hidden risks in common prescriptions, to knowing which medications to question or avoid altogether. You’ll see how liver disease affects dosing, how Medicare substitution rules can accidentally hurt seniors, and why removing personal info from pill bottles isn’t just about privacy—it’s about safety. This isn’t about scaring you. It’s about giving you the tools to ask the right questions, spot red flags, and keep your loved ones—or yourself—safe while taking the meds they need.
Cumulative Anticholinergic Burden: How Antihistamines Combine with Other Medications to Risk Cognitive Decline
Cumulative anticholinergic burden from antihistamines and other medications increases dementia and fall risks in older adults. Learn how to spot hidden drug interactions and switch to safer alternatives.
read more