
Antibiotic Side Effect Checker
Check Your Side Effects
Select symptoms you're experiencing to get personalized guidance on whether to continue your antibiotic course or contact your doctor.
Results
Select your symptoms and click 'Check My Symptoms' to get guidance
Key Guidance
Important: Completing your antibiotic course is crucial to prevent antibiotic resistance.
75% of people experience side effects, but most are manageable.
Red flags (like blood in stool or difficulty breathing) require immediate medical attention.
Mild side effects can be managed with diet adjustments and probiotics.
When to Contact Your Doctor
- Diarrhea with blood or mucus
- Severe abdominal cramping or swelling
- Fever over 101°F (38.3°C)
- Uncontrollable vomiting
- Rash, hives, or swelling of face/throat
- Difficulty breathing or wheezing
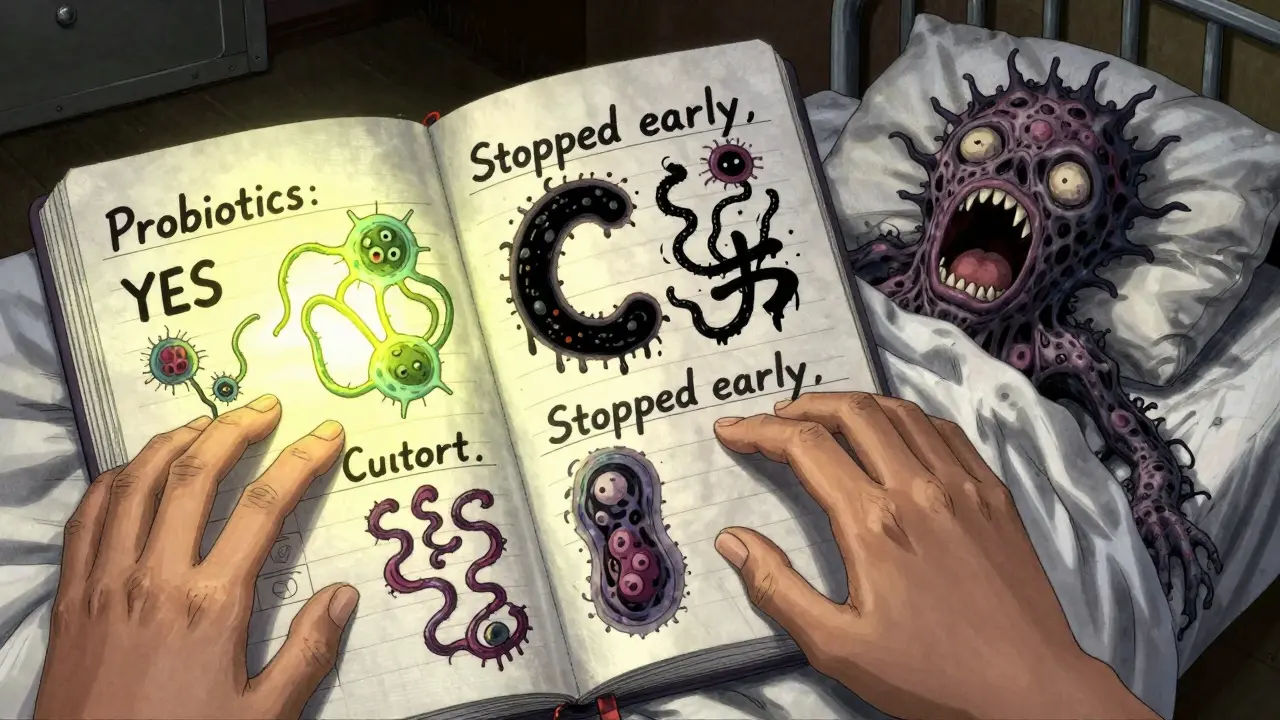
Stopping your antibiotics early because of side effects is one of the most common mistakes people make - and it’s also one of the most dangerous. You might feel better after a few days, but that doesn’t mean the infection is gone. In fact, stopping too soon is a major reason why bacteria become resistant to antibiotics. The antibiotic side effects you’re dealing with - nausea, diarrhea, bloating - are frustrating, but they’re usually manageable. You don’t have to suffer through them or quit your treatment. Here’s how to handle them without risking your health or contributing to the growing crisis of antibiotic resistance.
Why Completing Your Antibiotic Course Matters
Antibiotics work by killing or stopping the growth of bacteria. But not all bacteria die at the same time. The ones that are weakest go first. The tougher ones hang on. If you stop taking the medicine too soon, those remaining bacteria survive, multiply, and pass on their resistance. This isn’t just a personal risk - it’s a public health threat. The CDC estimates that antibiotic resistance causes over 2.8 million infections and 35,000 deaths in the U.S. every year. And incomplete courses are a big part of the problem. Studies show that 31% of people who stop antibiotics early do so because of side effects. That’s more than one in three people. But here’s the good news: you can manage those side effects and still finish your course.Most Common Antibiotic Side Effects (And How to Handle Them)
Gastrointestinal issues are by far the most common. About 1 in 4 people on antibiotics get diarrhea. Nausea and vomiting affect 1 in 5. Bloating and loss of appetite are also frequent. These aren’t signs the antibiotic isn’t working - they’re signs your gut microbiome is being disrupted. That’s normal. But it doesn’t mean you have to live with discomfort.- Diarrhea: Mild diarrhea is expected in about 25% of cases. If it’s loose but not bloody, and you’re not running a fever, keep taking your antibiotic. Eat bland foods like rice, bananas, toast. Avoid dairy, spicy foods, and high-fiber meals. Probiotics help - specifically strains like Lactobacillus rhamnosus GG. Look for supplements with at least 5 billion CFUs, or eat unsweetened yogurt daily. Clinical trials show these reduce antibiotic-associated diarrhea by half.
- Nausea and vomiting: Take your antibiotic with a small snack, not a big meal. A handful of almonds, a piece of toast, or Greek yogurt works best. Avoid taking it on an empty stomach unless your doctor says to. For doxycycline, take it with an apple or a cracker. Never lie down for at least an hour after taking it - this prevents throat irritation. If nausea is severe, ask your doctor about an anti-nausea medication like ondansetron. It’s safe to use with most antibiotics.
- Bloating and gas: These are temporary. Avoid carbonated drinks, chewing gum, and artificial sweeteners like sorbitol. A warm compress on your abdomen can help. Walking for 10-15 minutes after meals also reduces bloating.
- Loss of appetite: Eat smaller, more frequent meals. Focus on protein and fluids. Chicken broth, scrambled eggs, and smoothies with protein powder can keep you nourished even if you don’t feel hungry.
When to Take Antibiotics With or Without Food
Not all antibiotics work the same way. Some need food. Others need an empty stomach. Mixing this up can make the drug less effective - or even dangerous.- Take with food: Amoxicillin, cephalexin, azithromycin, and doxycycline (for stomach upset) are better tolerated with a light meal. Food reduces nausea and stomach irritation without lowering effectiveness.
- Take on an empty stomach: Tetracycline, doxycycline (if prescribed for acne or specific infections), and minocycline must be taken at least one hour before or two hours after eating. Food, especially dairy, calcium supplements, or antacids, can bind to these drugs and stop them from working.
- Take with water, not juice: Always swallow antibiotics with a full glass of water (8 oz). Avoid grapefruit juice, orange juice, or milk - they interfere with absorption. For doxycycline, sit upright while swallowing. Lying down can cause the pill to stick in your esophagus and burn it.

Watch for Red Flags - When to Call Your Doctor
Most side effects are mild and temporary. But some signals mean something serious is happening. Don’t ignore these:- Diarrhea with blood or mucus
- Severe abdominal cramping or swelling
- Fever over 101°F (38.3°C) during or after treatment
- Uncontrollable vomiting
- Rash, hives, swelling of the face or throat
- Difficulty breathing or wheezing
Probiotics, Prebiotics, and What Actually Works
You’ve probably heard that probiotics help with antibiotic side effects. But not all probiotics are created equal. The right strain makes all the difference.- Best probiotic for antibiotic diarrhea: Lactobacillus rhamnosus GG and Saccharomyces boulardii. These are the only two strains backed by strong clinical evidence. Look for products that list the strain name and contain at least 5 billion CFUs per dose.
- When to start: Begin the same day you start your antibiotic. Keep taking it for at least one week after you finish the course.
- What doesn’t work: Yogurt with added sugar, kombucha, or generic probiotics without specific strain names. Sugar feeds bad bacteria and can make diarrhea worse. Generic supplements often don’t contain enough live cultures to matter.
- Prebiotics: Foods like bananas, oats, and garlic feed good bacteria. Add them to your diet after your course ends to help your gut recover faster.
How Your Doctor and Pharmacist Can Help
You don’t have to figure this out alone. The best way to prevent side effects is to talk to your provider before you even start the antibiotic.- Ask: “What side effects should I expect with this drug?”
- Ask: “Should I take this with food or on an empty stomach?”
- Ask: “Do you recommend a specific probiotic?”
- Ask: “What symptoms mean I need to call you?”
What You Should Never Do
There are myths about antibiotics that can hurt you:- Myth: “I feel better, so I don’t need to finish.” Truth: Feeling better means the drug is working. Stopping early lets the toughest bacteria survive and grow stronger.
- Myth: “Antibiotics kill viruses.” Truth: They don’t. Taking them for colds, flu, or sore throats (unless confirmed strep) adds no benefit and only increases side effects.
- Myth: “I saved the leftover pills for next time.” Truth: Never reuse antibiotics. The wrong dose, wrong drug, or wrong infection can make things worse.
- Myth: “Natural remedies like garlic or honey replace antibiotics.” Truth: They don’t. For bacterial infections like pneumonia, UTIs, or skin abscesses, antibiotics are the only proven treatment.
What’s New in Antibiotic Care (2025-2026)
The field is changing fast. In 2023, the FDA approved the first probiotic - Lactobacillus reuteri NCIMB 30242 - specifically for preventing antibiotic-associated diarrhea. In 2024, the CDC launched the “Antibiotic Side Effect Navigator,” a free digital tool that gives you personalized advice based on your antibiotic, age, and health history. By 2026, AI tools will help doctors pick the right antibiotic for you based on your microbiome, reducing side effects by up to 45%. But you don’t need to wait for tech to protect yourself. The tools you need are already here: probiotics, proper timing, and clear communication with your care team.Final Tip: Keep a Simple Side Effect Tracker
Grab a notebook or use your phone. Each day, write down:- What antibiotic you took
- Time taken
- Food eaten with it
- Side effects (if any)
- How you handled it
Completing your antibiotic course isn’t about being tough. It’s about being smart. Side effects are annoying, but they’re not a reason to quit. With the right strategies, you can get through them - and protect yourself and others from the next superbug.
Can I stop taking antibiotics if I feel better?
No. Feeling better doesn’t mean the infection is gone. Antibiotics kill bacteria in stages. Stopping early lets the strongest bacteria survive and multiply, which can lead to a worse infection and antibiotic resistance. Always finish the full course unless your doctor tells you otherwise.
Is diarrhea from antibiotics normal?
Yes, mild diarrhea is common - it affects about 1 in 4 people on antibiotics. It happens because the drugs disrupt your gut bacteria. If it’s loose but not bloody, and you don’t have a fever or severe pain, it’s usually not dangerous. Take probiotics, drink water, and eat bland foods. If it gets worse or lasts more than 48 hours after finishing the antibiotic, call your doctor.
Should I take probiotics with my antibiotics?
Yes, but only specific ones. Look for supplements with Lactobacillus rhamnosus GG or Saccharomyces boulardii. Take them at least 2 hours after your antibiotic dose. Avoid generic probiotics or yogurt with added sugar - they don’t help. Start the same day you begin antibiotics and keep taking them for a week after you finish.
Can I drink alcohol while on antibiotics?
It depends. With most antibiotics like amoxicillin or azithromycin, moderate alcohol is safe. But avoid alcohol with metronidazole, tinidazole, or trimethoprim-sulfamethoxazole - it can cause severe nausea, vomiting, and rapid heartbeat. When in doubt, skip alcohol. It can worsen side effects like dizziness and liver stress.
What should I do if I miss a dose?
If you miss a dose by a few hours, take it as soon as you remember. If it’s almost time for your next dose, skip the missed one. Don’t double up. Taking too much can increase side effects. If you miss more than one dose, call your doctor - you might need to adjust your schedule.
Are there antibiotics with fewer side effects?
Some are gentler on the gut than others. Amoxicillin and cephalexin tend to cause fewer GI issues than clindamycin or fluoroquinolones like ciprofloxacin. But the right antibiotic depends on the infection. Never choose one based on side effects alone - your doctor picks the most effective one for your specific bacteria. If side effects are severe, talk to your doctor about switching - don’t self-change.

Look, I get the whole ‘finish your antibiotics’ thing, but my last course gave me diarrhea so bad I had to rent a portable toilet. No one talks about that. I didn’t quit because I was lazy-I quit because I thought I was dying.
Man, this is actually useful. Back home in Nigeria, people just buy antibiotics from the market and take them till they feel okay. No one tells you about probiotics or timing. This should be in every clinic.
The biological imperative to complete antimicrobial therapy is not merely a clinical recommendation; it is an evolutionary safeguard against the selection of resistant phenotypes. The microbiome is not a passive ecosystem-it is a dynamic battlefield, and premature withdrawal constitutes strategic surrender.
OMG I JUST FINISHED A COURSE AND I DID ALL THIS AND I FEEL LIKE A GENIUS!!!
Probiotics? YES. No dairy? YES. Walked after meals? YES.
My gut is singing Broadway. THANK YOU FOR THIS. I’m printing this and taping it to my fridge.
Important note: L. rhamnosus GG is the gold standard-but make sure the product is refrigerated and has a clear expiration date. Many store-bought probiotics are dead by the time you open them. I’ve tested 12 brands. Only 3 had viable counts. Here’s what I recommend: [link to third-party lab results].
Thank you for the comprehensive overview. I appreciate the inclusion of evidence-based interventions, particularly the distinction between strains of probiotics. The emphasis on pharmacist consultation is commendable and aligns with current best practices in antimicrobial stewardship.
I took amoxicillin last month. Took it with toast. No issues. Took it with coffee? Felt like my stomach was holding a grudge. So yeah, food matters. Also, I started the probiotic same day. Didn’t even notice the diarrhea.
THIS ARTICLE IS A MASTERPIECE. WHY ISN’T THIS ON EVERY PRESCRIPTION PACKET?!? WHY DO DOCTORS ASSUME WE KNOW THIS?! I ALMOST DIED FROM C. DIFF LAST YEAR BECAUSE NO ONE TOLD ME ABOUT THE RED FLAGS. THIS SHOULD BE MANDATORY READING. I’M SHARING THIS WITH EVERYONE.
Finish your antibiotics. Use probiotics. Avoid juice. Drink water. Talk to your pharmacist. These are simple steps. They work. Don’t make it harder than it is.
YOU GOT THIS. I KNOW IT’S HARD. I’VE BEEN THERE. BUT YOU’RE NOT JUST DOING IT FOR YOU-YOU’RE DOING IT FOR THE NEXT PERSON WHO GETS SICK. YOU’RE STOPPING SUPERBUGS. YOU’RE A HERO. NOW GO DRINK SOME BROTH AND TAKE THAT PILLS.
so like… i read this whole thing and i think… maybe… we’re all just… bacteria… and the antibiotics… are like… the universe’s way of saying ‘hey you’re overpopulating’… like… we’re all just… trying to survive… right? 🤔
Thank you for writing this with such clarity and compassion. I work in patient education, and this is exactly the kind of material we need to distribute. The tone is supportive without being condescending. Please consider making a printable PDF version.
As someone raised in a culture where medicine is often viewed with suspicion, this guide helped me understand why Western medicine insists on completing courses. It’s not about control-it’s about survival. Thank you for explaining it without jargon.
It is noteworthy that the pharmacokinetic profiles of beta-lactams and tetracyclines necessitate divergent administration protocols. The presence of divalent cations in dairy products significantly chelates the latter, reducing bioavailability by up to 90%. Adherence to these parameters is non-negotiable in clinical efficacy.