Every year, millions of Americans rely on generic drugs to manage chronic conditions like high blood pressure, diabetes, and thyroid disorders. These medications are supposed to be cheaper versions of brand-name pills - same active ingredient, same effect, lower cost. But over the last decade, what was once a reliable way to save money has turned into a financial rollercoaster. Some generic drugs dropped in price by 80% or more. Others jumped 1,000% overnight. And for many people, the cost of their monthly prescription has become unpredictable - sometimes unaffordable.
How Generic Drug Prices Have Changed Since 2013
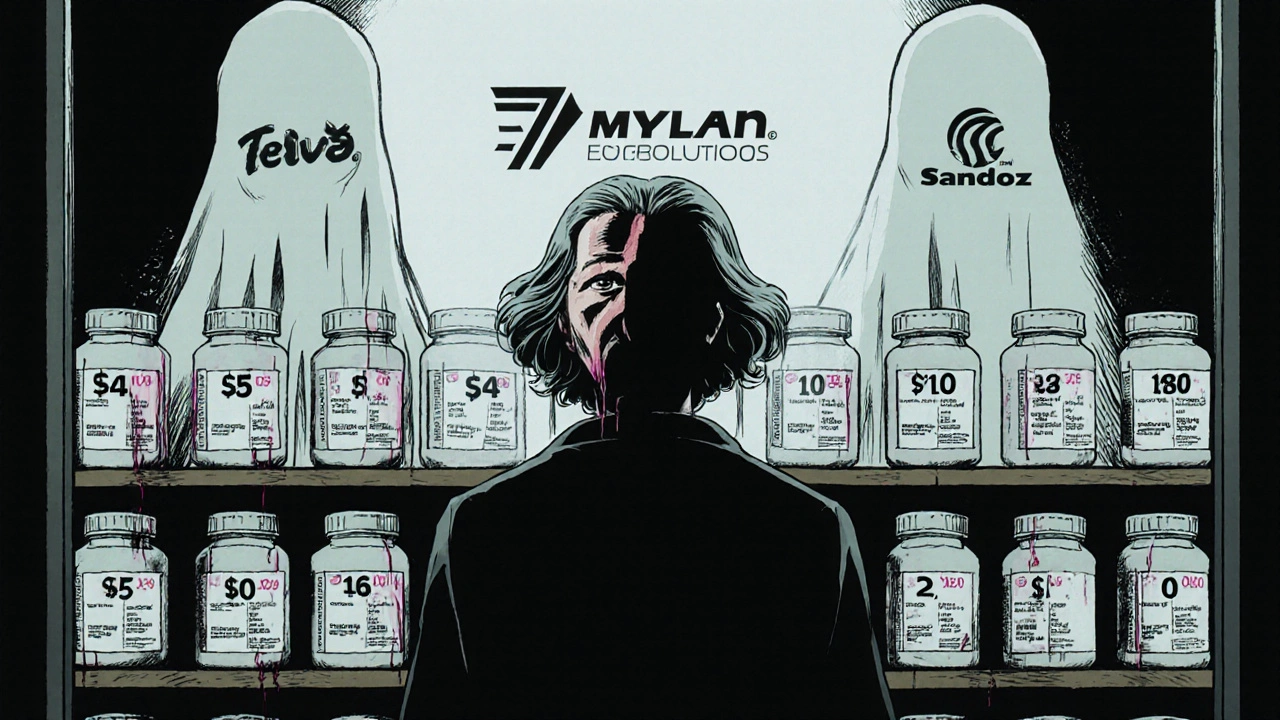
In 2013, the generic drug market looked very different. There were more manufacturers making the same pills, competition was fierce, and prices kept falling. But things started to shift. By 2018, the number of companies making generic drugs had dropped from 150 to just 80. A few big players - like Teva, Mylan, and Sandoz - now control most of the market. When only one or two companies make a drug, they can raise prices without fear of losing customers.
Take nitrofurantoin, a common antibiotic for urinary tract infections. Between 2013 and 2018, its price jumped 1,272%. That’s not a typo. A pill that cost $0.15 in 2013 was selling for nearly $2 by 2018. Meanwhile, levothyroxine, a thyroid hormone replacement, dropped 87% over the same period. Why the difference? It’s not about the drug’s effectiveness. It’s about how many companies make it. Levothyroxine had dozens of manufacturers. Nitrofurantoin had only two.
According to FDA data, when five or more companies make a generic drug, prices fall to about 15% of the original brand-name cost. But when only one or two companies are left, prices hover around 70-90% of the brand. That’s why some generics are dirt cheap - and others are shockingly expensive.
Year-by-Year Price Shifts: The Real Numbers
Looking at the data from 2019 to 2024, generic drug prices don’t move in a straight line. They jump, dip, and sometimes vanish - then reappear at double the cost.
- 2019-2020: Prices fell overall as more generics entered the market after patent expirations. The FDA approved over 800 new generic applications in 2020 - a record. Savings for consumers hit $11 billion that year.
- 2021-2022: Prices started to climb. A 2022 analysis found that 40 generic drugs saw price hikes averaging 39%. One of them? Furosemide, a diuretic used for heart failure. Its price jumped 150% in just 12 months.
- 2023: The average list price for generics rose 4.9%, the slowest increase in five years. But that average hides the truth. About 15% of generics had price changes over 20%. Some spiked over 100%. Others dropped just as sharply.
- 2024: Medicaid rules changed in January, removing a cap on rebates. This forced some brand-name drug makers to lower prices - but had little effect on generics. Instead, supply chain issues became the main driver of price swings. A single factory shutdown in India or China can cause a drug to disappear from shelves - and reappear at 200% higher cost.
Here’s what that looks like in real life. A patient taking generic lisinopril - a blood pressure pill - paid $4 a month at Walmart in early 2022. By late 2023, the same prescription cost $45. That’s a 247% increase. And it’s not rare. GoodRx data shows similar spikes for at least 20 other common generics in the same timeframe.
Why Do Prices Spike So Wildly?
It’s not just greed. It’s a broken system.
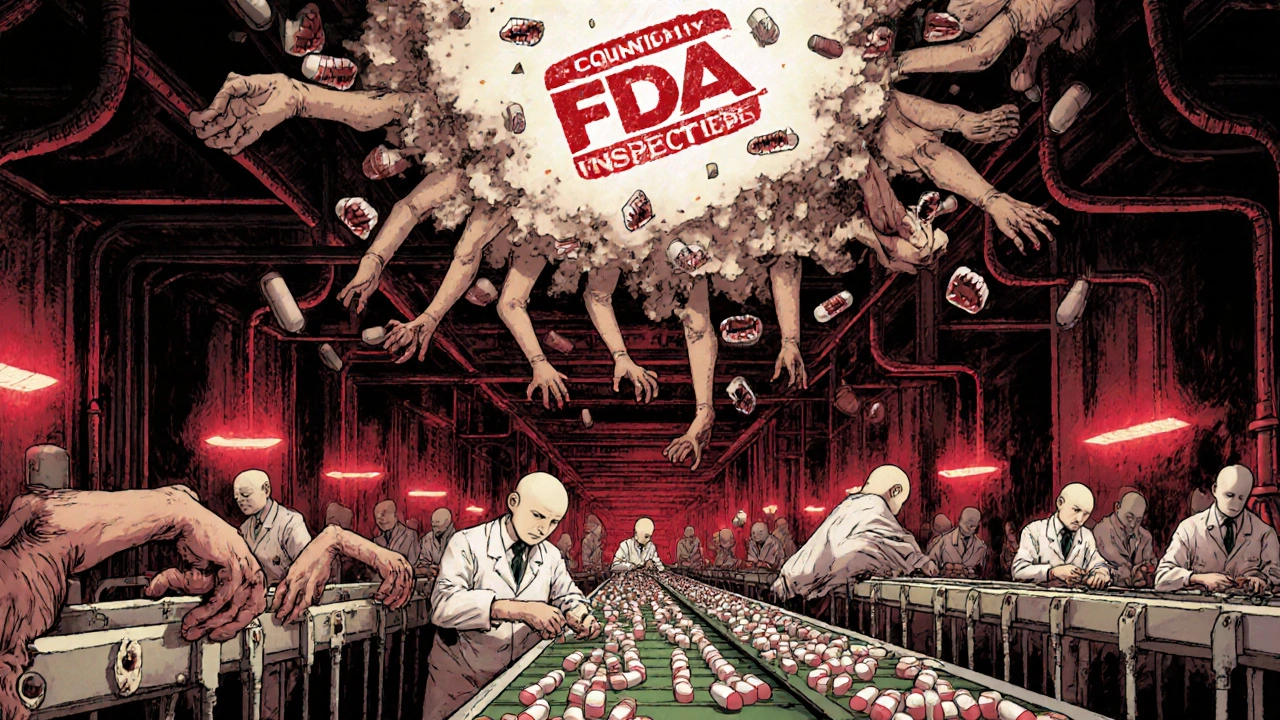
Most generic drugs are made overseas. In 2023, the FDA found quality issues in 23% of foreign manufacturing plants. When one plant fails inspection, production stops. If that plant was the only one making a certain drug, the supply vanishes. Manufacturers can’t just crank out more pills overnight. It takes months to get FDA approval for a new facility. In the meantime, prices skyrocket.
Another problem: consolidation. The top five generic drug makers now control over half the U.S. market. That’s up from 38% in 2015. Fewer companies mean less competition. And less competition means less pressure to keep prices low.
Then there’s the Medicaid Best Price rule. It forces manufacturers to give the lowest price they offer to any buyer - including Medicaid - to all others. So if a company gives a deep discount to a big pharmacy chain, they have to offer it to everyone. That makes it risky to lower prices at all. Many manufacturers just keep prices high to avoid being forced into losses.
And don’t forget the supply chain. A single shipment delay from India can cause a nationwide shortage. In 2022, the HHS found that 35% of generic drug shortages were directly tied to price increases over 50%. The average shortage lasted over six months.
Who Gets Hurt the Most?
It’s not the big insurers or the hospitals. It’s the people paying out of pocket.
A 2024 survey by KFF found that 37% of Medicare beneficiaries taking generic medications skipped doses or cut pills in half because they couldn’t afford them. That’s nearly four in ten seniors managing chronic illness - choosing between food, rent, or their medicine.
Independent pharmacies are suffering too. Forty-two percent of small pharmacies reported margin compression on 15% of their generic inventory. Some drugs went from being profitable to losing money in weeks. One pharmacist in Ohio told Drug Topics: “I had to stop stocking generic metformin because I was losing $2.50 on every script. I couldn’t afford to keep it.”
Meanwhile, patients using tools like GoodRx are still saving money - on average, $112.50 per prescription. But those savings only work if the drug is available. When it’s not, GoodRx can’t help. And when prices jump, even the best coupon won’t make a $50 pill affordable.
What’s Being Done - and What’s Not
The government knows there’s a problem. The FTC has 12 active investigations into unjustified price hikes in generic markets with few competitors. The FDA has a new plan to speed up approvals for drugs made by only one or two companies. And the Inflation Reduction Act now requires brand-name drug makers to pay rebates if their prices rise faster than inflation.
But none of that directly fixes the core issue: too few manufacturers, too much concentration, and zero safety net when supply breaks.
The Congressional Budget Office estimates that generic drug prices will grow just 1.5% per year through 2030 - far slower than brand-name drugs. That sounds good. But that average hides the 15% of generics that are “high vulnerability” to sudden spikes. Those are the ones that break budgets and force people to choose between pills and groceries.
Experts like Dr. Aaron Kesselheim from Harvard say the solution isn’t more regulation - it’s more competition. “We need to make it easier for new companies to enter the market,” he says. “Right now, the barriers are too high. The FDA can approve a drug in 10 months. But getting a factory built, inspected, and approved? That takes three years.”
What You Can Do Right Now
If you’re paying for generics out of pocket, here’s what actually works:
- Check GoodRx or SingleCare. Prices vary wildly between pharmacies. A $40 script at CVS might be $12 at Walmart or $8 at Costco.
- Ask for a 90-day supply. Many pharmacies offer discounts for larger quantities. You might pay $20 for three months instead of $15 a month.
- Call your pharmacy and ask why the price changed. Sometimes, they can reorder from a different distributor. Don’t accept “that’s just the price.”
- Switch to a different generic brand. Not all lisinopril is the same manufacturer. One brand might be $5. Another might be $45. Ask your pharmacist which one they’re dispensing.
- Use mail-order services. Many insurers offer lower prices through mail-order pharmacies. You might get three months of pills for the cost of one.
And if your price jumps more than 50% in a year - especially if you’re on Medicare or Medicaid - file a complaint with your state’s insurance commissioner. These spikes aren’t normal. They’re the result of market failure. And they’re becoming more common.
The Bigger Picture
Generic drugs save the U.S. healthcare system over $250 billion a year. That’s money that goes to hospitals, doctors, and patients. But if the system keeps breaking down - if a life-saving pill suddenly costs ten times more - then those savings vanish.
The goal of generics was simple: make medicine affordable. For most drugs, it still works. But for too many, it doesn’t. And the ones that don’t? They’re the ones that keep people from getting better.
Why do generic drug prices change so much from year to year?
Generic drug prices change because of supply and demand, competition, and manufacturing issues. When multiple companies make the same drug, prices drop. When only one or two are left, they can raise prices. Factory shutdowns, FDA inspections, and supply chain delays also cause sudden spikes. About 15% of generics experience price changes over 20% each year - often because of these disruptions.
Are generic drugs always cheaper than brand-name drugs?
Yes - but not always by much. Most generics cost 80-85% less than the brand-name version. However, in markets with little competition, a generic can cost 70-90% of the brand price. In rare cases, when supply is cut off, a generic can even cost more than the brand for a short time.
Which generic drugs are most likely to have price spikes?
Drugs with only one or two manufacturers are the riskiest. Cardiovascular drugs like nitrofurantoin, furosemide, and digoxin, and central nervous system drugs like levetiracetam and phenytoin have had the worst price spikes. These are often older drugs with low profit margins - so few companies want to make them. When one quits, prices jump.
Can I get a cheaper price by switching pharmacies?
Absolutely. Pharmacy pricing for generics varies wildly. A prescription that costs $50 at CVS might be $12 at Walmart or $8 at Costco. Always compare prices using apps like GoodRx or SingleCare before filling your prescription. Even small changes in the manufacturer can mean big price differences.
Why aren’t generic drug prices regulated like brand-name drugs?
Brand-name drugs are now subject to inflation rebates under the Inflation Reduction Act. But generics aren’t - because they’re supposed to be competitive by nature. The system assumes that more manufacturers = lower prices. But when competition disappears, there’s no legal mechanism to stop price gouging. That’s why regulators are now looking at antitrust violations in concentrated generic markets.
If you’re struggling to afford your medication, talk to your doctor. They may be able to prescribe an alternative with a more stable price - or help you find patient assistance programs. You’re not alone. And you don’t have to accept price hikes as normal.

bro i paid $4 for lisinopril last year now its $45 at walmart 😭 my dog gets cheaper meds than me
It is unconscionable that pharmaceutical monopolies are allowed to exploit vulnerable populations under the guise of 'market forces.' This is not capitalism-it is predation dressed in corporate suits. The FDA must enforce antitrust statutes immediately, not issue press releases.
15% of generics spike over 20%? That’s the tip of the iceberg. The real problem is the 70% of generics made in one factory in India. One power outage. One FDA violation. Boom. Your blood pressure med vanishes. And no one in DC cares until someone dies. This system is a time bomb wired to your pill bottle.
just called my pharmacy. they said the manufacturer changed and the new batch costs 3x more. asked if they could order from another distributor. they shrugged. guess im just supposed to pay it.
as someone who lived in India for five years and saw generic drug factories up close-this isn’t just about greed. It’s about infrastructure collapse. The same plants that make your metformin also make malaria meds for Africa. When global supply chains get strained, the cheapest drugs are the first to vanish. We need to treat pharmaceutical manufacturing like critical infrastructure-not a profit center.
i started using GoodRx last year and saved over $800 on my meds. but when the drug is just gone? no app helps. i had to go without my thyroid med for three weeks last winter. i felt like a ghost. people need to know this isn’t rare-it’s routine now.
you think this is accidental? nah. the same people who own the big pharma companies also own the FDA contractors. they let one factory fail so the others can raise prices. watch. next year the price of nitrofurantoin drops again-right after a new 'independent' company 'enters the market.' same owners. same playbook.
oh no, poor baby. you can't afford $45 for a pill? maybe don't live in a country where you expect healthcare to be affordable. go to Thailand. it's $2.50 there. problem solved. also, stop using apps. just buy the brand name. you're clearly rich enough to complain about it.
lol who even uses generics anymore? just get the brand. its like $10 more a month. big deal. also i heard the FDA is just fake anyway. they take bribes from china. also i saw a guy on youtube say the pills are laced with rat poison now. just saying.
you’re not alone. i had to switch from lisinopril to benazepril last year because the price went nuts. my pharmacist helped me find a cheaper brand. it’s the same thing, just different name. ask your doc. they’ve seen this before.
why do some generics have 20+ manufacturers and others have one? is there a pattern based on drug class or patent expiration timing? i’m trying to understand the selection bias.
The Congressional Budget Office’s projection of 1.5% annual growth for generic drug prices is statistically misleading. It obscures the fact that 15% of drugs experience volatility exceeding 100%. This is not a trend-it is systemic instability. Policy must target concentration, not averages.
Let me offer some context. The U.S. healthcare system operates under a complex web of incentives that disincentivize competition in the generic space. The FDA approval process, while rigorous, is not optimized for rapid entry. Meanwhile, Medicaid’s Best Price rule, intended to ensure equity, inadvertently discourages price reductions by creating liability for manufacturers. To truly fix this, we must decouple pricing from reimbursement structures and incentivize multi-source production through tax credits and expedited review pathways. It’s not just about regulation-it’s about reengineering the entire ecosystem.
my neighbor died last month because she couldn’t afford her heart meds. they went from $12 to $90 in six months. she cut pills in half. then she stopped taking them. the obituary didn’t mention it. no one talks about it. but i’m talking now. this is murder by bureaucracy.